The cases
In 2011, two cases of NNT were reported from the paediatric unit of Port Moresby General Hospital (PMGH) and one case of NNT was reported from Rumginae Rural Hospital (RRH) in Western Province of Papua New Guinea. The two PMGH cases resided in Goilala district, central Province and the Rumginae case in Middle Fly district, Western Province (Figure 1). Middle Fly is characterized by forests, swamps, rivers and coast, and access is predominantly by dugout canoes, outboard powered dinghies and aircraft due to the vastly scattered villages being separated by large bodies of water.9 The average household size of Middle Fly district is 6.8; 89% of the population are reside in traditional dwellings, and 87% of the population are engaged in agriculture as the principal economic activity.10 The Goilala district is a remote district characterized by very rugged topography with more than 70% comprised of deeply dissected valleys and mountains.11 There is no road access to the Goilala district from provincial headquarters in Port Moresby, and the communities are usually serviced by light aircraft landing on treacherous mountain top airstrips.11 TT vaccine coverage for women of childbearing age (WCBA) in Goilala and Middle Fly districts were low at 9% and 12%, respectively, in 2011.

Figure 1. Map of the location of neonatal tetanus cases, Papua New Guinea, 2011
All three cases (two males and a female) were delivered at home on the floor, and the births were attended by untrained assistants (Table 1). The umbilical cord was cut in two of these cases with a bush knife, while in the other an old razor blade was used. The umbilical cords in these three cases were tied with strings from a rope, a rice bag and a grass skirt. All three babies were reportedly normal at birth and had normal crying and sucking for the first two days of life. All three babies started having difficulty in sucking after two days, and they developed symptoms of convulsions and spasms at an average of eight days after birth. The youngest of the multi-gravidae mothers was 16 and the eldest 29 years. Only one of the mothers received any antenatal care or TT vaccination in her past pregnancies, while none of these mothers received any antenatal care or TT vaccination in the current pregnancy. The two cases that were admitted to PMGH survived, while the case at RRH died three days after admission to the hospital; there was no fatality among the mothers. Follow-up of the cases discharged from PMGH was not possible due to the geo-topography of their residential location; hence, no comment can be made on the final clinical outcome in regards to neurological and developmental status of these cases after discharge.
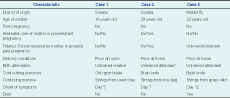
Table 1. Characteristics of mother and births for the three neonatal tetanus cases, Papua New Guinea, 2011
The policy
The confirmation and detailed investigation of these three cases by hospital physicians in 2011, along with the reported suspected cases of NNT by the health workers through the syndromic surveillance system, led to the drafting of the National Action Plan for Elimination of Maternal and Neonatal Tetanus in Papua New Guinea.12 The action plan targeted WCBA (15–45 years) for three rounds of nationwide supplementary immunization activities with TT. This is in line with the WHO position paper on tetanus.13 A “high-risk approach” to control NNT in countries where the elimination target (< 1 case per 1000 live births at the district level) has not yet been reached. This high-risk approach should be targeted towards all WCBA and immunization doses must be delivered using a campaign-style immunization programme of three doses of TT with an interval of at least four weeks between doses one and two and of at least six months between doses two and three. Strengthening other measures to prevent MNT in the country, including clean delivery, training of midwives and community health workers ,and improvement in ante-natal care services, were also highlighted in the national elimination plan.
The first immunization round targeted 1.6 million WBCA and was conducted in April and May 2012. Around 1.3 million (77%) women were reached with the TT vaccine during the first round.14 This supplementary immunization campaign was administered using multiple approaches at fixed site (maternal and child health clinics at health centres, school vaccination sessions, markets and congregation site sessions), day mobile and overnight patrol outreach sessions. The second immunization round was conducted in October through December 2012; final coverage results are pending.
Discussion
These three NNT cases in Papua New Guinea must be viewed as sentinel events indicating a triple failure of public health in routine immunization, antenatal care and clean delivery/cord care services. Unsafe cord practices were evident in all three cases. As reported in Papua New Guinea as early as 1991, unsafe birth practices, including cutting the cord with sharpened sea shells, fresh bamboo knifes, metal blades or knifes, were common practices.15 Strengthening clean delivery practices is one component of the National Action Plan that aims to decrease the incidence of such unsafe practices. Following the introduction of a programme promoting clean delivery practices and the replacement of cow dung for postnatal umbilical cord care with clean water or milk in Kenya and Tanzania, there was significant reduction in annual NNT incidence. After introduction of the programme in 1981, NNT rates fell sharply, and by 1988 annual death rates had dropped to 0.75 per 1000 births in the intervention areas compared with 82 per 1000 in control areas. These changes were both culturally acceptable and safer alternatives.16
Although cases of NNT have been reported every year in the National Health Information System, it was the reporting and confirmation of the these three NNT cases by physicians at PMGH and RRH that led to the formulation of the National Action Plan for Elimination of Maternal and Neonatal Tetanus in Papua New Guinea. In order to achieve the elimination of MNT in Papua New Guinea, the other components of the National Action Plan need to be implemented, including the third and final immunization round, the strengthening of clean delivery practices and NNT surveillance. More detailed investigations of NNT cases reported in the health information system as well as sub-provincial analyses following completion of all three immunization rounds should be conducted.
Conflicts of interest
None declared.
Funding
None.
References:
- Roper MH, Vandelaer JH, Gasse FL. Maternal and neonatal tetanus. Lancet, 2007, 370:1947–1959. doi:10.1016/S0140-6736(07)61261-6 pmid:17854885
- Wassilak SGF et al. Tetanus Toxoid. In: Plotkin SA, Orenstein WA (eds). Vaccines, 4th edition. Philadelphia, WB Saunders Publishing, 2004, 745-781.
- Okan M et al. Long-term neurologic and psychomotor sequelae after neonatal tetanus. Journal of Child Neurology, 1997, 12:270–272. doi:10.1177/088307389701200410 pmid:9203069
-
Data on Neonatal Tetanus. Reported incidence time series: WHO Immunization surveillance, assessment and monitoring. Geneva, World Health Organization, 2012. Available from: http://www.who.int/immunization_monitoring/data/data_subject/
en/index.html [accessed 30 November 2012]. -
WHO-recommended standards for surveillance of selected vaccine-preventable diseases. Geneva, World Health Organization, 2003. Available from: http://whqlibdoc.who.int/hq/2003/WHO_V&B_03.01.pdf [accessed
30 November 2012]. -
The Partnership, Maternal and Neonatal Tetanus Elimination. Geneva, World Health Organization, 2012. Available from: http://www.who.int/immunization_monitoring/
diseases/MNTE_initiative/en/index1.html [accessed 30 November 2012]. -
Ministerial Taskforce Report on Maternal Health in Papua New Guinea. Waigani, National Department of Health, 2009. Available from: http://www.unfpa.org/sowmy/
resources/docs/library/R149_DOH_PNGUINEA_2009_Ministerial_Taskforce_report_
final_version_3.pdf [accessed on 30 November 2012]. - National Annual Sector Performance Review. Waigani, Papua New Guinea National Health Information System, 2012.
- Learn about Western Province and Papua New Guinea, 2012. Available from: http://www.otdfpng.org/learn [accessed on 30 November 2012].
-
Papua New Guinea 2000 Census provincial report. Waigani, National Statistical Office of Papua New Guinea, 2010. Available from: http://www.spc.int/prism/
country/pg/stats/2000_Census/census.htm [accessed 30 November 2012]. - Climate and Weather Goilala. Available from: http://goilala.com/people-and-place/climate-weather [accessed 30 November 2012].
- National Plan of Action for Maternal and Neonatal Tetanus Elimination, Papua New Guinea, 2012–2014. Port Moresby, National Epidemiology Unit, 2011.
- Tetanus vaccine. Weekly Epidemiological Record, 2006, 81:198–208. pmid:16710950
- Report on Integrated Measles Supplementary activity 2012. Waigani, Epidemiology Unit, Public Health Division, National Department of Health.
- Taylor P et al. Mother Care country assessment. Papua New Guinea, May 1991.
- Meegan ME et al. Effect on neonatal tetanus mortality after a culturally-based health promotion programme. Lancet, 2001, 358:640–641. doi:10.1016/S0140-6736(01)05787-7 pmid:11530155