a Public Health Unit, South Western Sydney Local Health District, New South Wales, Australia.
Correspondence to Leng Boonwaat (email: leng.boonwaat@sswahs.nsw.gov.au).
To cite this article:
Boonwaat L et al. Underreporting of influenza outbreaks in aged care facitilities in South Western Sydney, Australia, 2014. Western Pacific Surveillance and Response Journal, 2016, 7(1):31–33. doi:10.5365/wpsar.2015.6.3.001
In 2014, influenza activity was high in New South Wales (NSW), Australia, and 21 443 people were hospitalized with a diagnosis of influenza-associated pneumonia. This translates to a rate of 252.4 cases per 100 000 population. More than 18 000 cases of laboratory-confirmed influenza were reported in NSW. The majority were influenza A, dominated by A/H3N2 subtype. There were also 111 influenza outbreaks in aged care facilities (ACFs) reported in NSW in 2014, the highest number on record.1
Elderly residents in ACFs experience high rates of morbidity and mortality during influenza outbreaks. They are at increased risk of developing complications due to underlying diseases.2 These residents also have an increased risk of infection because of the institutional environment they share with many other residents and staff. Furthermore, impaired oral intake, limited dexterity and altered consciousness may limit treatment options when they are infected.3
The Australian Government’s Department of Health and Ageing (DHA) has issued specific guidelines for prevention and control of influenza outbreaks in residential care facilities.4 While ACFs have primary responsibility for managing outbreaks, Public Health Units (PHUs) are required to promote ACF compliance with these guidelines and facilitate delivery and administration of antivirals. However, effective influenza prophylaxis and other timely interventions can only occur if PHUs are notified in a timely manner.5
DHA guidelines indicate influenza outbreaks in ACFs are to be reported to PHUs.4 However, under NSW public health legislation, reporting of outbreaks in ACFs is not mandatory.6 In this report we investigated whether there were outbreaks that were not reported to the South Western Sydney Local Health Districts PHU during the 2014 influenza season.
Influenza is a laboratory-notifiable disease in NSW.7 Influenza cases are confirmed by viral culture or polymerase chain reaction from nasopharyngeal aspirates or nose and throat swabs. In ACFs, samples are taken by either nursing staff or attending medical officers or taken during hospital admission. Results are electronically notified to the NCIMS from corresponding laboratories.
DHA guidelines4 define an influenza outbreak as:
ILI is defined as sudden onset of fever (body temperature ≥38 °C) plus cough and/or other respiratory symptoms (e.g. shortness of breath) plus one or more systemic symptom(s) (fatigue, muscle soreness, headache).
For a conservative estimate, we use three or more confirmed cases of influenza in residents or staff of the facility (by either laboratory or point-of-care test) to define an influenza outbreak for analysis.
Notifications of influenza among residents of South Western Sydney Local Health District that were reported to the NCIMS during 2014 were extracted and stratified by age. Those aged 65 years or above were selected for further analysis. The selected cases with residential addresses corresponding to the ACFs in NSW were identified. These ACFs were then cross-referenced with a database of influenza outbreaks reported to the PHU in 2014 for comparison. Data analysis was conducted using the Statistical Analysis Software (SAS Institute, Cary, North Carolina, USA).
Informal interviews with facility managers were conducted by PHU staff on an ad hoc basis to understand the managers’ knowledge of outbreak recognition and what factors should trigger a notification.
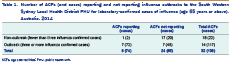
The results revealed that 139 of 549 laboratory-confirmed influenza cases aged 65 years or above had originated from 32 known ACFs. Eight ACFs with one or more confirmed cases (range 2–16 cases) reported their cases to the PHU. Twenty-four ACFs with one or more confirmed cases did not report their cases to the PHU (range 1–16 cases). There were 14 ACFs with three or more confirmed cases of influenza. Only seven of them (50%) reported the influenza outbreaks appropriately (Table 1). A delay of one to four days occurred between onset of ILI and notification to the PHU.
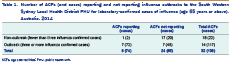
ACFs, aged care facilities; PHU, public health unit.
Informal interviews were conducted with managers from five ACFs that reported ILI among residents before June 2015. Results revealed that although all managers (n = 5) were aware of the need to report an outbreak, some were unsure what number of cases constituted an outbreak and others did not know when to report. In some cases, managers believed they had to wait for the laboratory confirmation before notifying the PHU. High workload was also a reason given for delays in reporting.
The results revealed that half of ACFs that should have reported an influenza outbreak did not do so. This is similar to a British survey where only 20% (n = 34) of all local Health Protection Units were formally notified of ILI occurring within ACFs.8
It is unclear whether ACFs were cognizant of the influenza outbreak definition in the DHA guidelines.4 Feedback from facility managers indicated that various factors could have contributed to delays in notification. Nonetheless, delays in identification and notification of influenza outbreaks in ACFs have led to difficulties in containing the spread of influenza. These challenges with influenza outbreak reporting are not unique to the South Western Sydney Local Health District. Other PHUs have reported fear of bad publicity as another reason for delays in notification by ACFs.9 Factors such as awareness of outbreak definitions and the assumption that laboratory confirmation should occur before notification can be corrected with improved education and training provided by the PHU before the annual influenza season.
Limitations of the study include the reliance on information provided by facility managers with potential recall bias and laboratory reporting. Unreported outbreaks of ILI may have occurred for which laboratory testing was never done. Also, reported ACF outbreaks of ILI may never be classified as influenza outbreaks because of insufficient testing. PHU staff do not have the resources to routinely conduct onsite investigations and testing for every reported ACF outbreak of ILI.
The study suggests that PHUs should ensure that ACFs understand the DHA guidelines, specifically the importance of the epidemiological link between cases and influenza outbreaks. Reminders and education sessions should be issued to ACFs before the beginning of influenza seasons to ensure ACF facility managers are able to recognize outbreaks and provide timely notifications to PHUs. Furthermore, it may be useful for PHUs to conduct influenza preparedness activities, possibly in the form of desktop exercises.
None declared.
None.
The authors would like to acknowledge all PHU staff involved in managing ACF-based influenza outbreaks.