a Hunter New England Local Health District, New South Wales, Australia.
b Health Protection New South Wales, North Sydney, New South Wales, Australia.
c Sydney Local Health District, Camperdown, New South Wales, Australia.
d South Western Sydney Local Health District, Liverpool, New South Wales, Australia.
Correspondence to Tony Merritt (email: Tony.Merritt@hnehealth.nsw.gov.au).
To cite this article:
Merritt T et al. Effect of antiviral prophylaxis on influenza outbreaks in aged care facilities in three local health districts in New South Wales, Australia, 2014. Western Pacific Surveillance and Response Journal, 2016, 7(1):14–20. doi:10.5365/wpsar.2015.6.3.005
Background: There was a record number (n = 111) of influenza outbreaks in aged care facilities in New South Wales, Australia during 2014. To determine the impact of antiviral prophylaxis recommendations in practice, influenza outbreak data were compared for facilities in which antiviral prophylaxis and treatment were recommended and for those in which antivirals were recommended for treatment only.
Methods: Routinely collected outbreak data were extracted from the Notifiable Conditions Information Management System for two Local Health Districts where antiviral prophylaxis was routinely recommended and one Local Health District where antivirals were recommended for treatment but not routinely for prophylaxis. Data collected on residents included counts of influenza-like illness, confirmed influenza, hospitalizations and related deaths. Dates of onset, notification, influenza confirmation and antiviral recommendations were also collected for analysis. The Mann–Whitney U test was used to assess the significance of differences between group medians for key parameters.
Results: A total of 41 outbreaks (12 in the prophylaxis group and 29 in the treatment-only group) were included in the analysis. There was no significant difference in overall outbreak duration; outbreak duration after notification; or attack, hospitalization or case fatality rates between the two groups. The prophylaxis group had significantly higher cases with influenza-like illness (P = 0.03) and cases recommended antiviral treatment per facility (P = 0.01).
Discussion: This study found no significant difference in key outbreak parameters between the two groups. However, further high quality evidence is needed to guide the use of antivirals in responding to influenza outbreaks in aged care facilities.
Influenza is a notifiable condition in New South Wales (NSW), Australia. Aged care facilities (ACFs) are encouraged to notify influenza outbreaks to their local public health unit (PHU), where they are recorded in the NSW Notifiable Conditions Information Management System (NCIMS). There were 111 influenza outbreaks notified in NSW ACFs during 2014, the highest on record (Figure 1).1 Notified influenza outbreaks require at least one laboratory-confirmed case. The predominant circulating influenza strain in 2014 was A(H3N2). As there was a relatively poor match between the circulating and the seasonal influenza vaccine strain in that year,2 an effective antiviral intervention would have been particularly valuable for influenza outbreak control.
ACF, aged care facility.
There is inconsistent international guidance on the role of antivirals during influenza outbreaks in ACFs, and practice varies both in Australia and internationally. The Communicable Disease Network of Australia guidelines note that “there is a potential role for antiviral medications in the management of influenza outbreaks in residential care facilities as an adjunct to other control measures”,3 and Victorian Health guidelines note that “prophylaxis may be recommended in some cases”.4 In contrast, antiviral treatment and prophylaxis are routinely recommended for ACF influenza outbreaks in Canada5 and the United States of America6 based mainly on the findings of observational studies7–11 and a randomized controlled trial (RCT) of seasonal prophylaxis.12
The significant resource implications when considering antiviral prophylaxis, including the costs of health staff and medication, further support the need for a strong evidence base for prophylactic antiviral use. To determine the impact of antiviral prophylaxis recommendations in practice, influenza outbreak data were compared for facilities in which antiviral prophylaxis and treatment were recommended and for those in which antivirals were recommended for treatment only.
NSW is divided into 15 Local Health Districts (LHDs), each with a PHU. A convenience sample of two LHDs in which antivirals were routinely recommended to ACFs with influenza outbreaks for both treatment and prophylaxis (prophylaxis group) and one LHD in which antivirals were routinely recommended to ACFs for treatment only (treatment-only group) were included in the analysis.
All facilities were provided with routine outbreak management and infection control advice in accordance with Australian guidelines at the time of notification.3 In the prophylaxis group, antiviral treatment and prophylaxis were recommended after the first influenza case was confirmed. The PHU sent a letter to the ACF to inform attending medical officers about the outbreak and to recommend oseltamivir treatment for symptomatic cases within 48 hours of onset. Prophylaxis was recommended to other residents for 10 days or until the outbreak was declared over, whichever was the longer period.3 If the outbreak was confined to a section or wing that was reasonably separate from the remainder of the facility, a recommendation to offer prophylaxis only to residents in that area was made on some occasions. If ACFs did not have ready access to oseltamivir, a starter pack was provided by the PHU. Prophylaxis was routinely recommended for staff at one LHD.
In the treatment-only group, antiviral treatment of cases, in accordance with national guidelines,3 was discussed with ACF staff when the first confirmed case was notified. Routine response measures for both groups included: isolation of ill residents, exclusion of ill staff, cohorting staff to work with either ill or well residents, limiting admission of new residents for the duration of the outbreak, use of appropriate personal protective equipment and enhanced cleaning.
All influenza outbreak data for 2014 were extracted from the NCIMS database, including the outbreak details, facility characteristics and key response features (Table 1). All confirmed influenza cases in the outbreaks were positive by polymerase chain reaction at a laboratory accredited by the National Association of Testing Authorities.13 Only illness in residents (but not in health-care workers) was included in the analysis.
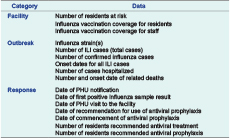
ILI, influenza-like illness; and PHU, public health unit.
Outbreak duration, attack rate, hospitalization rate and case fatality rate were calculated for each facility. Attack rate was further assessed for two time periods: before and after PHU notification. To assess the timeliness of PHU notification, the time from the earliest instance of three influenza-like illness (ILI) cases within a 72 hour period (a potential influenza outbreak)3 to PHU notification was calculated. The time from notification to laboratory confirmation of influenza and the earliest time at which prophylactic antiviral use could be considered was also determined. When confirmation occurred before notification, this period was recorded as zero days. Definitions for the key analysis terms are listed in Table 2.

ILI, influenza-like illness; and PHU, public health unit.
Median and interquartile values were calculated for relevant outbreak parameters and the Mann–Whitney U test was used to assess the significance of differences between group medians. Differences are reported as significant for P < 0.05. Stata version 11 (StataCorp LP, Texas, USA) was used for all calculations.
The ACFs in the treatment-only and in the prophylaxis groups had comparable numbers of residents at risk (median 85.0 versus 87.5 residents, P = 0.92). Influenza vaccination rates for the two groups did not differ significantly for staff (50.0% versus 39.0%, P = 0.11) or for residents (95.6% versus 98.0%, P = 0.23) (Table 3).
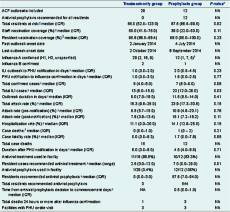
* Mann–Whitney U test was used.
† One outbreak had both influenza A H1 and H3 strains confirmed.
‡ Per facility.
ACF, aged care facility; ILI, influenza-like illness; IQR, interquartile range; NA, not applicable; and PHU, public health unit.
A total of 41 outbreaks were included in the analysis. The treatment-only group had 29 confirmed influenza outbreaks notified during 2014, affecting 22.1% of the 131 ACFs in the district. Antiviral prophylaxis was used for three residents who shared a room with a confirmed case in one large outbreak in this group (with 22 cases and 120 residents at risk). This outbreak was retained as the antiviral prophylactic usage was minimal.
The prophylaxis group had a total of 13 confirmed influenza outbreaks in 2014, affecting 6.2% of the 210 ACFs in the two districts (6/63, 9.5% and 7/147, 4.8% in each LHD, respectively). In three outbreaks, prophylaxis was recommended for only part of the ACF resident population. Twelve outbreaks were included in the analysis after excluding one outbreak that was notified too late for prophylaxis.
Influenza was laboratory confirmed in 47.3% and 41.2% of the ILI cases in the treatment-only and prophylaxis groups, respectively. The number of confirmed cases per facility was lower in the treatment-only group than the prophylaxis group (median 5 versus 7, P = 0.06) as was the number of ILI cases in each outbreak (median 13 versus 23, P = 0.03) (Table 3).
Both groups had a similar mix of implicated influenza strains. Influenza A was identified in all outbreaks. The predominant strain was A/H3N2. Influenza B was also identified in two outbreaks in the treatment-only group and one in the prophylaxis group (Table 3). Four outbreaks had two different influenza strains identified (two in the treatment-only and two in the prophylaxis group). All outbreaks in the prophylaxis group and 89.7% (26/29) of outbreaks in the treatment-only group occurred during the influenza season from July to September 2014. Oseltamivir was used for treatment and prophylaxis in all outbreaks.
The outbreak duration (median 9.0 days versus 11.5 days, P = 0.41), overall attack rate (18.3% versus 23.9%, P = 0.15), hospitalization rate (11.1% versus 14.1%, P = 0.15) and case fatality rate (0.0 versus 1.7, P = 0.95) were all lower in the treatment-only group than the prophylaxis group, but the differences were not statistically significant. There was also no significant difference between the two groups in pre- and post-notification attack rates or in outbreak duration after notification (P > 0.05) (Table 3).
The time from meeting the Communicable Disease Network of Australia’s potential influenza outbreak criteria3 to PHU notification was similar for the treatment-only and prophylaxis groups (median 1 day versus 2 days, P = 0.23), as was the time from notification to confirmation (median 1 day versus 1.5 days, P = 0.77). For three outbreaks in the prophylaxis group, influenza confirmation occurred before PHU notification. The median time from antiviral prophylaxis recommendation to medication commencing was 0.5 day (interquartile range, 0.0–1.0 day) for the prophylaxis group.
Based on the available data, antivirals were used for treatment in a lower proportion of facilities in the treatment-only group (68.8% versus 83.3%), and fewer cases per facility were treated with antivirals in the treatment only group (2.5 versus 7.0 cases, P = 0.01) (Table 3).
We found no significant difference in outbreak attack rate, duration, hospitalization or case fatality rate for those ACFs recommended antiviral treatment alone compared to those recommended antiviral treatment and prophylaxis. The facilities in the two groups had similar numbers of residents and comparable vaccination coverage for both residents and health workers. All outbreaks in the study occurred in NSW during 2014, with the majority in the three-month period between July and September.
The results are consistent with a recent European RCT in an aged care setting14 that found no evidence that antiviral prophylaxis during an influenza outbreak reduced the risk of new infections over a four-year period; however, the European study was underpowered. In contrast, an Australian RCT concluded that there was “some support for a policy of treatment and prophylaxis with oseltamivir in controlling influenza outbreaks in ACFs”,15 but the authors in that study also noted that the trial lacked power. Concerns were subsequently raised that one of the three control outbreaks in that study, in which there was a delayed and incomplete intervention, should be excluded. With that outbreak removed, the apparent beneficial effect of antiviral prophylaxis disappeared.16 A subsequent review by the Academy of Medical Sciences in the United Kingdom in 2015 concluded that there was inadequate evidence to “inform a single approach for prophylaxis in care homes” and that “further research is needed to inform decisions on whether or not to use [antivirals] in prophylaxis in care homes”.17
Some important potential confounding factors were considered in our analysis, including differences in the timeliness of notification, outbreak severity and the thoroughness of interventions between the two groups. No significant difference in the timeliness of PHU notification between the two groups was identified. Outbreak severity was assessed in several ways in this study. The attack rate for the period up to notification did not differ significantly between groups, which is consistent with the two groups having similar overall severity. However, there were some other indications that outbreaks may have been more severe in the prophylaxis group, with median values for overall attack rate and hospitalization rates higher than in the treatment-only group, although neither was significantly different.
A higher proportion of facilities in the treatment-only LHD reported having influenza outbreaks in 2014. There may have been more outbreaks in this district or there may have been relative underreporting of outbreaks in the prophylaxis districts. An audit of laboratory notifications for influenza in one LHD in the prophylaxis group identified seven ACFs with three or more linked cases of confirmed influenza and a further 15 facilities with one or two cases of confirmed influenza that did not report an outbreak to the PHU in 2014 (South Western Sydney LHD, unpublished data, 2014). Data were not available to assess whether non-reported outbreaks were less severe than those that were notified.
There was also limited capacity to assess the thoroughness of interventions. The same national response guidelines3 were used for general infection control advice, but it was not possible to further explore the comparability and completeness of interventions at ACFs. Detailed data on non-antiviral outbreak measures and the extent to which antiviral recommendations were implemented by ACFs were not available. Additional information on antiviral use in future influenza seasons would enhance the analysis of routinely collected ACF outbreak data.
We found four outbreaks had two different influenza strains, indicating multiple importations into those facilities. Other outbreaks may have had unidentified multiple importations with potential impact on the course of the outbreak. Influenza was confirmed in less than half of the ILI cases in the treatment-only and prophylaxis groups. Some residents with ILI may have been infected with other pathogens that affected the analysis.
This was an observational study and is subject to several limitations. The use of antiviral prophylaxis was neither randomized nor blinded, and systematic differences between groups could have confounded the analysis. Notification timeliness, outbreak severity and thoroughness of intervention have been considered in detail, and the overall outbreak profile was similar for the two groups. However some parameters were not considered, including staff illness data, the outbreak setting (some occurred in high dependency units or semi-independent hostel settings), residents’ demographics and co-morbidities and the overall resident acuity.
Our analysis did not find evidence that a policy of recommending prophylactic antivirals in ACF influenza outbreaks reduced attack rate, outbreak duration, hospitalization rate or case fatality rate during the 2014 influenza season in NSW. Despite the study limitations, the absence of any differences between groups suggests that any effect of antiviral prophylaxis in practice is likely to have been small or negligible. There is a need for further high quality evidence to guide use of antivirals in influenza outbreak response in ACFs.
None declared.
None.
The authors would like to acknowledge the many public health staff from the Hunter New England, Sydney and South Western Sydney Public Health Units and all of the aged care facility and laboratory staff who were involved in the identification and management of these outbreaks.