a Department of Health, Sta Cruz, Manila, Philippines.
b Mogpog Municipal Health Office, Marinduque, Philippines.
Correspondence to Ray Justin Ventura (e-mail: rayjustinventura@gmail.com).
To cite this article:
Ventura RJ et al. A community-based gastroenteritis outbreak after Typhoon Haiyan, Leyte, Philippines, 2013. Western Pacific Surveillance and Response Journal, 2015, 6(1):1–6. doi:10.5365/wpsar.2014.5.1.010
Background: Three weeks after Typhoon Haiyan, an increasing number of acute gastroenteritis cases were reported in Kananga, Leyte, an area where evacuated residents had returned home two days after the disaster. An outbreak investigation was conducted to identify the source and risk factors associated with the increase of gastroenteritis.
Methods: A case was defined as any person in Kananga who developed acute diarrhoea (≥ 3 times/24 hours) and any of the following symptoms: fever, nausea, vomiting or abdominal pain from 11 November 2013 to 10 December 2013. Active case finding was conducted by reviewing medical records, and a case-control study was conducted. Rectal swabs and water samples were tested for bacteriological examination.
Results: One hundred and five cases were identified. Multivariate analysis revealed that consumption of untreated drinking-water was associated with illness (adjusted odds ratio: 18.2). Both rectal swabs and municipal water samples tested positive for Aeromonas hydrophila. On inspection of the municipal water system, breaks in the distribution pipes were found with some submerged in river water.
Conclusion: This acute gastroenteritis outbreak was most likely caused by Aeromonas hydrophila and transmitted through a contaminated water source. This study highlights that areas less damaged by a disaster that do not require ongoing evacuation centres can still have acute gastroenteritis outbreaks. All affected areas should be monitored during a disaster response, not just those with evacuation centres. Boiling or chlorinating of water should also be recommended for all areas affected by disaster.
Typhoon Haiyan swept through the central Philippines on 8 November 2013, killing over 6000 and displacing 4 million people; it damaged schools, health centres, other infrastructure and 1.1 million houses.1
In western Leyte, the typhoon affected 18 municipalities with a total of 884 546 people affected. Unlike other areas affected by the typhoon, evacuation centres in Kananga, Leyte, decamped two days after the typhoon with all evacuees returning to their own houses. Although western Leyte appeared to have suffered less than eastern Leyte and Samar,1 a lack of disease surveillance reports from this area was a concern. Therefore, active surveillance was established at the Kananga Municipal Hospital and Kananga Rural Health Unit, which reported on vector-borne diseases, tetanus and diarrhoea.
Three weeks after Typhoon Haiyan, an increasing number of acute gastroenteritis cases were reported in Kananga, Leyte, through this active surveillance system. The 60 cases reported in November 2013 were 757% higher than the same month the previous year.2 Therefore, a team from the Department of Health was sent to conduct an outbreak investigation to identify the source and risk factors associated with the increase of gastroenteritis.
A case was defined as any person in Kananga, Leyte with acute diarrhoea (≥ 3 times/24 hours) and any of the following signs and symptoms: fever, nausea, vomiting and abdominal pain from 11 November to 10 December 2013. Active case finding was conducted by reviewing medical records from Kananga Rural Health Unit and Kananga Municipal Hospital. The initial 10 cases were interviewed using a structured questionnaire which included questions on food and water exposures and other environmental risk factors. A map showing attack rates and water supply by village was constructed using ArcGIS (Redlands, CA, USA).
An unmatched case-control study with a planned 1:2 ratio of cases to controls was conducted to test the hypothesis. Not all cases were included due to logistical barriers with purposive selection of cases. Controls were individuals who resided in the same or nearby households to the case; they were excluded if they reported any gastrointestinal symptoms or if they tested positive from bacterial examination. A more specific questionnaire was used for the case-control study that focused on drinking-water, hygiene practices and other environmental factors. These exposures were then compared, and analysis was conducted using EPI info version 3.5.4. We calculated odds ratios (OR) and confidence intervals. A forward stepwise procedure was used in developing a model for the multivariate analysis which included variables that were significant in the bivariate analysis.
Rapid diagnostic test was conducted using Denka (Japan) for rotavirus and CTK (San Diego, CA, USA) for norovirus. Rectal swabs were collected for both cases and controls, as well as for a family that was living near the water supply, using Cary-Blair media for standard bacterial culture testing.
A single water sample (500 ml) was collected from each of the three intake tanks and two reservoirs of the municipal water system. Six water sources connected to the municipal water system were chosen purposively for collection of a single water sample (500 ml) (Village Poblacion, Village Natubgan and Village Lonoy). The specimens were sent to Research Institute for Tropical Medicine, Mutinlupa City, the Philipines for bacterial analysis. The Swiss humanitarian aid team, which was conducting relief efforts after Typhoon Haiyan, also tested three water sources connected to the municipal water system for residual chlorine (Reservoire, Village Natubgan and Village Poblacion)
Environmental investigation was conducted in the three villages with the highest number of cases that were using the municipal water system.
A total of 105 cases were identified. The first onset date was 11 November 2013 with a peak from 17 to 20 November (Figure 1). The majority (101 or 96%) reported watery diarrhoea with four cases (4%) reporting bloody diarrhoea. Other signs and symptoms included vomiting (51%), fever (47%) and abdominal pain (32%). Forty-eight cases (46%) were hospitalized and no deaths were reported. Nineteen of the cases reported antibiotic use before laboratory testing.
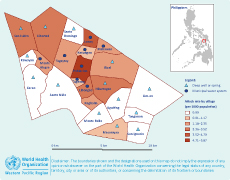
The age of cases ranged from 4 months to 61 years (median = 2 years) with 51% male. The most affected age group was 1 to 5 years (49%). Poblacion village had the highest attack rate (AR) (AR = 6/1000 population) followed by Barangay Lonoy (AR = 4.46/1000 population), both of which were supplied water through the municipal water system (Figure 2). Twenty-five out of 39 cases interviewed used the municipal water system; 72% were not disinfecting the water.
The case-control study comprised 39 cases and 61 controls. None of the 61 selected controls tested positive on bacterial examination. Bivariate analysis revealed three significant risk factors: drinking untreated water (not chlorinated or boiled, mostly municipal water), no access to toilet facilities and using deep wells or springs as a drinking-water source. After multivariate analysis, only drinking untreated water remained associated with being a case and the adjusted OR of 18.17 was similar to the crude OR of 22.15 (Table 1).
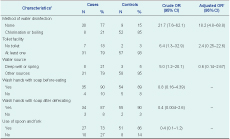
* Totals may not add up due to missing responses.
† Also adjusted by age and sex.
CI, confidence interval; OR, odds ratio.
The four specimens tested for rotavirus and norovirus were negative. Of the 39 rectal swab specimens collected for cases, 11 (28%) were positive for the following bacterial pathogens: Aeromonas hydrophila (four or 10%), Campylobacter jejuni (three or 8%), Campylobacter coli (three or 8%) and Shigella sonnei (one or 3%).
All 61 controls selected had negative rectal swabs for bacterial culture. All four cases that tested positive for Aeromonas hydrophila had the municipal water system as their source of drinking-water. A total of 11 water samples were collected and three (27%) were positive for Aeromonas hydrophila (two intake tanks of the municipal water system and a household in Village Natubgan). No residual chlorine was detected in the three water sources tested.
Eight of the 22 villages used the municipal water supply which, since 2012, has been manually disinfected with chlorine granules twice-weekly. This application was not interrupted after the typhoon. However, the quantity and frequency of chlorine application was based on previous practices, and the amount used was not computed based on the approximate volume of water in the tank. There was no data on the capacity of the reservoir or the current level of water. Water testing through primary health care media was irregularly done due to lack of kits. There was no routine bacteriological or physicochemical examination of any drinking-water sources.
Several damaged main distribution pipes of the system were fixed after three to four days. However, upon inspection of the municipal water system during the outbreak investigation, breaks in the distribution pipes were found with some of these submerged in river water. The intake tanks with manual chlorinators were also inspected, and there were no chlorine granules left in the pail inside the tank. It was reported that the water system pressure was at 10 psi compared to an average of 20 psi, indicating leaks in the distribution system.
Also, after the typhoon, a family built a temporary shelter at the wall of one of the two reservoirs of the municipal water system. The family practised open defecation in the absence of a toilet facility. Rectal swabs from three of the asymptomatic children from this family were negative for bacteriological culture.
This acute gastroenteritis outbreak was most likely caused by Aeromonas hydrophila and transmitted through a contaminated water source. The fact that the same bacteria were found in the municipal water system and in cases provides strong evidence of the source of infection. The distribution of cases by village also shows that the highest attack rates were recorded in areas where their main source of drinking-water was the municipal water system; a high proportion of cases using the municipal water system reported not boiling or chlorinating their drinking-water. The case-control study showed a significant association between illness and consumption of untreated drinking-water, suggesting a waterborne source. Studies have proven that boiling or chlorinating is an effective way of disinfecting water.3,4
Aeromonas hydrophila is a gram-negative, facultatively anaerobic bacteria widely present in aquatic environments including drinking-water systems.5 The symptoms of aeromonas gastroenteritis are not easily distinguished from gastroenteritis of other causes.6,7 There have been several outbreaks caused by Aeromonas hydrophila mostly due to contaminated drinking-water and food. A recent outbreak involving 381 cases in a school in China identified Aeromonas hydrophila as the likely pathogen with environmental investigation, showing that the implicated vegetables were washed in polluted water from a tank close to a sewage ditch,8 similar to the suspected contamination in this study.
After the typhoon, some of the distribution pipes of the water system were broken; a drop in water pressure was also reported, indicating that not all breaks were fixed. These breaks may have been the entry point for the bacterial pathogen. Chlorine applied in the reservoir was inadequate after the typhoon, which most likely allowed the growth of the bacteria.
Aeromonas hydrophila was considered the cause of this outbreak; however, several cases tested positive for Campylobacter coli, Campylobacter jejuni and Shigella sonnei. These pathogens are more common in foodborne outbreaks, but they have also been linked to waterborne outbreaks.9,10 It is possible that these pathogens were present in the water supply, but as only 500 ml of water was collected per water source, this may not have been enough to detect their presence. Testing larger volumes of water is required to detect Campylobacter, with 4000 ml to 20 000 ml increasing the chance of detection.11 As these pathogens were not detected in the water, the investigation cannot rule out that these infections were due to a different source or that there was more than one outbreak occurring.
There are some limitations in this investigation, mostly due to the investigation being conducted during a disaster situation. During the case-control analysis, several questionnaires had incomplete responses, and there was a low positivity rate of testing, although this may be explained as 19 of the cases had already taken antibiotics before samples were collected. This study was not able to evaluate village-related risk factors because the choice of controls in the case-control study was matched by neighbourhood. Attack rates by village should also be interpreted with caution due to the lack of denominator stability in the post-typhoon setting.
In conclusion, this study was able to identify the likely source of the outbreak as evidenced by finding the same pathogen in both water and cases. The strong association with not chlorinating or boiling drinking-water (mostly from the municipal water supply) provides additional evidence that this was a waterborne outbreak. This study also shows that post-disaster, areas that are less damaged and that do not require ongoing evacuation centres, can still have acute gastroenteritis outbreaks. This suggests that during disaster response, all affected areas should be monitored, not just evacuation centres and that boiling or chlorinating water should be recommended for all areas affected by the disaster, even when supply systems are repaired. As part of a disaster response, all water systems should be monitored, repaired and protected from human contact. For this outbreak, we also recommend the procurement of a chlorinator machine for the municipal water system and regular monitoring of chlorine levels.
None declared.
This gastroenteritis outbreak investigation was funded by the Department of Health, Philippines.
We are grateful for the cooperation and support of the Center for Health and Development-Eastern Visayas, local government of Kananga, Kananga Municipal Hospital, Kananga Municipal Health Office and town residents during the field investigation. We also thank the laboratory staff of the Research Institute for Tropical Medicine for testing the samples.