a Mongolian Field Epidemiology Training Programme, Ulaanbaatar, Mongolia.
b National Center for Communicable Diseases, Ulaanbaatar, Mongolia.
c Health Department, Omnogovi Province, Mongolia.
d World Health Organization, Ulaanbaatar, Mongolia.
Correspondence to Jargalsaikhan Selenge (e-mail: seke_8@yahoo.com).
To cite this article:
Jargalsaikhan S et al. Investigation of a mumps outbreak in Mongolia, January to April 2011. Western Pacific Surveillance and Response Journal, 2012, 3(4):53–58. doi:10.5365/wpsar.2012.3.3.007
Introduction: The Gurvantes district in Omnogovi Province reported a suspected mumps outbreak to the Mongolia Ministry of Health in March 2011. An outbreak investigation team was established to verify the diagnosis and to determine the magnitude of the outbreak.
Methods: The descriptive study comprised retrospective investigation of local hospital medical records and surveillance data, and interviews with school teachers, doctors, probable cases and their close contacts. The World Health Organization standard case definition was used to define mumps cases. Clinical specimens were collected for laboratory confirmation.
Results: There were 153 cases, none under two years of age, with the five- to 14-years-old age group having the highest rates. There was no difference by sex (P = 0.12). A single index case appeared to be the source of the outbreak, and there were four outbreak waves. Of the 129 cases with information on epidemiological links, 94 (72.3%) were linked to other cases at a kindergarten or school, 17 (13%) were from secondary spread of family members, two (1.5%) were from secondary spread of other relatives, and 16 had no established links. Eight cases (5.2%) were confirmed through laboratory investigation.
Conclusion: This was the first high-magnitude mumps outbreak since the introduction of the measles-mumps-rubella vaccine in Mongolia in September 2009. There were no cases among vaccinated children; cases were seen among older children and adults not eligible for the vaccine. This suggests that immunity to mumps is still low in Mongolia. Future outbreaks may occur among this unvaccinated population.
Mumps is an acute viral disease caused by a paramyxovirus and is usually spread by respiratory droplets.1 Humans are the only natural hosts with one third of cases being asymptomatic. Infection typically begins with non-specific symptoms, such as myalgia, headache, malaise and low-grade fever, followed by unilateral or bilateral swelling of the parotid glands; unless complications occur the illness resolves completely.1,2 Orchitis, most commonly unilateral, occurs in 20%–30% of post pubertal male cases.2,2 Encephalitis and permanent neurological sequelae are rare complications. Pancreatitis is reported in approximately 4% of unvaccinated cases.3
Although mumps is most frequently reported in children aged five to nine years, both adolescents and adults may be affected. Children younger than 14 years comprise 90% of cases,4 and in countries that have not introduced mumps vaccine, 80%–90% of adults older than 20 years are immune from natural infection.2 One strategy to control mumps is to have the measles-mumps-rubella (MMR) vaccination as part of a national immunization programme.3 However, in recent years in countries with mumps vaccination, many mumps outbreaks have been identified among both vaccinated and unvaccinated people. Large mumps outbreaks were reported from Sweden in 2004,5 the United States of America in 2006,6 the Netherlands in 20107 among vaccinated populations and Scotland in 20108 where half the cases were vaccinated.
An early warning and response surveillance system consisting of case- and event-based surveillance was established in Mongolia in 2008. Mumps is one of the notifiable diseases reported to this system on a monthly basis by epidemiologists and health care providers from primary to tertiary level. Usually, mumps is confirmed clinically at the provincial level due to lack of laboratory capacity. Event-based surveillance is the organized and rapid capture of information about events that are a potential risk to public health such as a mumps outbreak. These outbreaks are required to be reported by the hospitals as soon as possible to the National Surveillance Unit of the National Centre for Communicable Diseases (NCCD).
Mumps vaccine was not available in Mongolia before 2009. Mumps epidemics occurred approximately every five years9 with 5073 mumps cases registered in 2006 and 1990 cases in 2009. The inter-epidemic years of 2007, 2008 and 2010 reported fewer than 1000 cases per year.9 Mumps vaccination was added to the routine vaccination schedule in September 2009 with two doses at nine and 24 months of age. The first dose is earlier than that recommended by the World Health Organization (WHO)3 due to many cases of mumps and measles being reported in Mongolia in the under one-year-old age group. In 2010, MMR vaccination coverage rates were 97% both at the national level and for Omnogovi Province.10 Therefore, in 2011, children aged between nine months to 3.5 years should have been protected by the vaccine with children older than 3.5 years old being susceptible.
An outbreak of suspected mumps was reported from the Gurvantes district to the NCCD, Ministry of Health in early March 2011. Fellows from the Mongolian Field Epidemiology Training Programme (MFETP) and staff from NCCD were invited by the Ministry of Health to investigate the outbreak.
A descriptive epidemiological study was conducted from 15 to 22 March 2011. The outbreak investigation team consisted of MFETP fellows, epidemiologists, a physician and a virologist of NCCD and the health department of Omnogovi Province.
Gurvantes district is located 300 km from the Omnogovi Province centre at the border with China and in 2011 had an official population of 4243. Trade across the border with China, as well as many mining and coal basin companies, are common in this district. There is frequent movement of the population between urban and rural areas.
Active case finding was conducted by the local health authority by screening all households on 7 March 2011. All outpatients and inpatients diagnosed with mumps in the Gurvantes district hospital were included in our survey. The probable and confirmed cases were based on the WHO-recommended case definition.11 A probable case was defined as any person who had “acute onset of unilateral or bilateral tender, self-limited swelling of the parotid or other salivary gland, lasting two or more days and without other apparent cause”11 in the Gurvantes district from 11 January to 8 April 2011. Confirmed cases were probable cases positive for mumps virus immunoglobulin M (IgM) on acute serum sample.
Data collection included: (1) synthesis of local hospitals’ medical records and surveillance data, (2) face-to-face interviews with cases and/or their relatives, and (3) interviews with school teachers and local doctors. The following data were collected: age, sex, social status, symptoms and complications, date of onset of illness and vaccination history. Population data were obtained from the local health government.
Attack rates (overall, by age, by gender) and frequencies were calculated using Epi-info. Epidemiological linkages, defined as a case who had been in contact with a probable or confirmed case during their incubation period (range 12–25 days from onset of symptoms),2 were also established among cases.
Samples were collected from probable cases from 16 to 18 March 2011. All serum samples were tested for the presence of mumps-specific IgM antibody using commercial enzyme immunoassays (NovaTec Immundiagnostic, Dietzenbach, Germany). Nested polymerase chain reaction (PCR) amplification of a 639 bp fragment encompassing the entire small hydrophobic gene was conducted. Positive PCR products were purified and sequenced. The nucleotide sequences were analysed with reference sequences of different genotypes to determine the genotype of the specimens.
Ethical clearance was not required as this outbreak investigation was considered to be a public health response.
There were 153 probable cases of mumps in the Gurvantes district between 11 January and 8 April 2011; an overall attack rate of 3.6%. Three cases were identified from medical records, seven through active surveillance and the remaining from the surveillance system.
Most cases had mild symptoms: swelling of salivary glands 152 (99%), fever 29 (19%), vomiting 23 (15%) and diarrhoea five (3%). Among the post pubertal males (> 17 years), six (33.3%) reported testicular pain. Twenty-four cases (16%) were hospitalized while the remaining 129 cases (84.3%) either sought outpatient treatment or self-medicated. There were nine cases (6%) with complications: meningitis (two cases), meningitis with orchitis (one case), orchitis (five cases) and pancreatitis (one case). Seven of these complicated cases were male. Eight of 12 serum samples were confirmed mumps-specific IgM antibody positive. In July 2011, the outbreak mumps virus genotype was identified as F type.
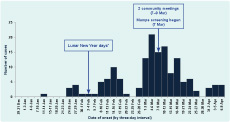
The epidemic curve shows that the onset date of the index case was 11 January 2011, and there were four outbreak waves. The first wave occurred at the end of January. Lunar New Year was celebrated from 2 to 5 February before the second and third wave of the outbreak. Community meetings, attended by most of the adults, were held on 7 and 9 March. On 7 March, household screening was conducted. The number of cases peaked at the end of March and returned to lower levels in April with the last case onset date of 13 April (Figure 1). The index case was identified as a student of a secondary school who had no travel history and could not recall any contact with any suspected mumps cases the month before onset of symptoms.
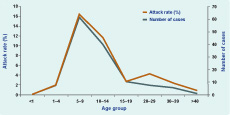
There were no cases among children aged less than 2.5 years old. The median age of cases was 10 years old (range: two to 40 years old) with about 70% of cases being children aged between five and 14 years old. A major proportion of cases (119, 78%) were children at kindergarten (under five years of age), elementary (six–10 years of age) and secondary schools (11–17 years of age); six (4%) cases were children who stay at home. The remaining 28 cases were adults (Figure 2). There was no significant difference of the attack rate between males and females (4% compared with 3%, respectively). All cases were unvaccinated.
Of the cases, 129 provided information about epidemiological linkages to other cases. Ninety-four cases (72.3%) had contact with another case at kindergarten or school, 17 cases (13%) were from secondary spread within households, two cases (1.5%) were linked to relatives; 16 cases (12.3%) had no identified exposures (Figure 3).
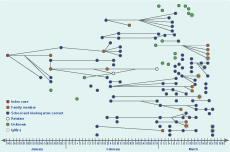
Note: Family member defined as person who lives in same house with contact. Relative defined as person who had visited contact’s house several times but does not live with contact.
This outbreak of mumps in the Gurvantes district from January to April 2011 is the first outbreak of mumps with high case numbers since the introduction of the MMR vaccine into the national immunization schedule in September 2009. The overall attack rate was 3.6%, much higher than recent reports in many other countries.12,13 This implies that the overall immunity level of the general population to mumps in Mongolia is low. There were no cases among children who were eligible for vaccination, and the attack rate was highest among the five- to 14-years-old age group, consistent with mumps cases reported in Mongolia from 2006 to 2010.9 This age group is unvaccinated and would not have natural immunity to mumps yet. The primary transmission of mumps in this outbreak was through kindergarten and school contacts.
Following the index case there were four outbreak waves with a generation period of about 20 days within three months. Generally the incubation period for mumps is 16–18 days (range: 12–25).9 Mongolian people celebrate Lunar New Year for three to five days. Relatives visit and are greeted with an arm-hold embrace. The community meetings would have been attended by most of the adult population. Those social activities could have facilitated the transmission of mumps and spread it to the community in the third and fourth generations of the outbreak. Another generation of the outbreak did not follow, possibly due to most adults having natural immunity to mumps. Testing identified mumps virus genotype F in this outbreak. Mumps virus genotype F circulated dominantly in China,14–16 a neighbouring country of Mongolia; transmission of mumps was possible between the two countries.
Six per cent of cases had a complication, consistent with published literature that reports mumps complications in 1.0%–10% of cases.24–,6 The five cases (28%) with orchitis were also similar to that reported previously at 20%–37% in adults.2,4,17 Recent mumps outbreaks in the vaccinated population reported lower percentages of mumps cases with orchitis, for instance, 5% in the United States of America in 2006,6 12% in the Netherlands in 20107 and 0.03% in Sweden in 2004.5
Our investigation had several limitations. There was a low proportion of laboratory confirmation (eight cases, 5.2%). However, the clinical symptoms of probable cases were consistent with mumps. The index case had no history of travel. It is likely that there were undetected cases in the district with mild symptoms or asymptomatic infections prior to the index case being detected. The number of cases could be underreported. Mass screening was conducted among the population during the investigation and so the possibility of missing cases would be minimal.
The investigation verified the outbreak and suggested that general immunity to mumps virus is still low among Mongolia’s young population despite the MMR vaccine being introduced into the national routine immunization programme in 2009. Health care workers should be aware that mumps outbreaks with high attack rates can occur among unvaccinated populations. All children’s institutions should report any child with mumps symptoms to the health organizations in a timely manner as an important action to control mumps. Since a single index case caused this outbreak, it is important to exclude people who have mumps symptoms from schools and workplaces. We also identified the need to conduct risk assessments on the probability of further spreading of mumps to other areas in the immediate future and for subsequent seasons.
None declared.
None.
We would like to thank the patients, clinicians and other staff of the Gurvantes district hospital; health department of Omnogovi Province, Mongolia; Viral Laboratory and Surveillance Department of NCCD; Dr G Surenkhand, NCCD Deputy Director for Communicable Diseases, Mongolia; and staff from the WHO Regional Office for the Western Pacific who conducted the scientific writing workshop.