a South Western Sydney and Sydney Local Health Districts Public Health Unit, New South Wales, Australia.
Correspondence to Kirsty Hope (e-mail: Kirsty.hope@sswahs.nsw.gov.au).
To cite this article:
Hope K et al. Measles transmission in health care waiting rooms: implications for public health response. Western Pacific Surveillance and Response Journal, 2012, 3(4):33–38. doi:10.5365/wpsar.2012.3.3.009
Background: Seventeen cases of locally acquired measles occurred in South Western Sydney and Sydney local health districts between July and October 2011. Three of the cases were known to have at least one dose of measles-mumps-rubella (MMR) vaccine. Seven cases were infected within a health care setting waiting room by five index cases. Current national protocols require follow-up of all susceptible contacts in the same waiting room for any length of time for up to two hours after the index case has left.
Methods: Cases were interviewed using a standardized questionnaire. Information included: demographics, illness and activities during the exposure and infectious periods. Health care settings provided arrival and discharge times, maps of floor layouts and location of patients during stay.
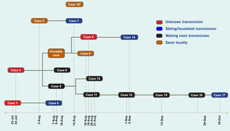
Results: All health care setting transmission occurred in cases who were present at the same time as their index cases, with cross-over time ranging from 20 to 254 minutes. No index case was isolated. Index cases were between day four and six of illness when transmission occurred. None of the five index cases and one of seven secondary cases had received at least one dose of MMR vaccine. Of the seven secondary cases, two were one year of age, one was 17 years old and four were between 30 and 39 years old.
Conclusion: As Australia moves towards measles elimination, follow-up of cases is important; however, with limited public health resources a targeted response is vital. In this small but well-documented series of secondary cases acquired in a health care setting, all were infected following direct, proximate contact of at least 20 minutes. Changes to the national guidelines may be warranted, ensuring that limited resources are focused on following up contacts at greatest risk of disease.
In countries close to achieving measles elimination, the epidemiology of reported measles cases has changed, with implications for public health and outbreak control. These changes include a shift in incidence from preschool-aged children to older age groups who may have missed vaccination as a child, an increasing proportion of international importations and an increasing pool of susceptible people among groups whose members do not routinely accept vaccinations such as those opposed to vaccination for religious or philosophical reasons.1,2 These changes in epidemiology and the infrequency of measles cases has allowed an increased focus on control of onward transmission settings where there is a high risk of measles transmission.3
Previous studies have shown that outside the home, measles is readily transmitted in educational facilities, sports halls, religious institutions, orphanages, refugee camps, aeroplanes and health facilities.4–8 Health facilities are of particular concern because of the risk of exposure to measles for those who may already be seriously ill. Health care waiting rooms in particular are important in the transmission of measles as a large number of sick and healthy people congregate together in a confined space.9
In countries where measles incidence is low, transmission is facilitated by failures or delays in diagnosis due to physicians inexperienced with an increasingly rare disease.10,11 This increases the likely number of presentations and time spent in waiting rooms. The importance of health care waiting rooms as a setting where measles transmission occurs is further enhanced by a failure to isolate the infectious patient or a lack of isolation facilities and low vaccination coverage of health care workers.11–14
Between July and October 2011, 17 cases of locally acquired measles occurred in South Western Sydney and Sydney local health districts. Seven secondary cases were infected within a health care setting waiting room by five index cases. Current Australian national protocols require follow-up of all susceptible contacts in the same waiting room for any length of time for up to two hours after the index case has left. People born before 1966 are ordinarily considered to be immune through natural infection, however, they are followed up to determine if they were accompanied by a person who may be at risk.13
In a metropolitan health authority that includes high demand emergency departments (EDs) and large general practices (GPs), adhering to the national protocol during an outbreak quickly consumes available public health resources. This paper describes the outbreak, transmission in health care settings and raises questions about the application of the national guidelines for public health response when resources are limited.
Analysis of a case series was conducted between July 2011 and January 2012. Cases were routinely notified by physicians or by laboratories as required by legislation.15 Cases were interviewed by a public health nurse using a standardized questionnaire. Information collected included: demographic details, onset date, symptoms, potential exposures and activities during the infectious periods. Public health action implemented in response to a confirmed case followed the New South Wales measles response guidelines.3 As part of the response to this outbreak GPs and EDs in the area were alerted and asked to report suspected measles to the Public Health Unit (PHU). For cases where transmission occurred in a healthcare setting waiting room (defined as either an ED or a GP waiting room), the facilities were contacted and asked to provide arrival and discharge times, maps of floor layouts and location of patients during their stay.
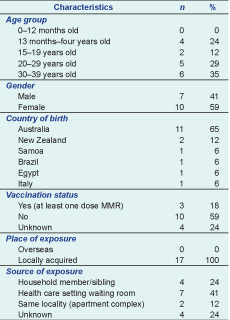
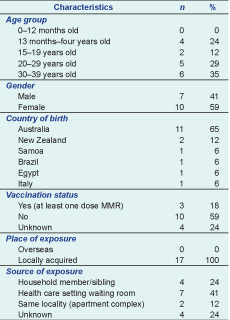
Seventeen cases of measles were notified to South Western Sydney (SW) PHU with an onset date between July and September 2011. Characteristics of the cases are outlined in Table 1. No case had travelled internationally in their exposure period or had contact with friends or family members who had recently travelled overseas. All cases were locally acquired, with seven acquiring their infection during a visit to a local ED or GP waiting room (Figure 1).
* In South Western Sydney and Sydney local health districts.
* South Western Sydney and Sydney local health districts.
† Case 10 acquired infection from a case who lives in another health jurisdiction.
All cases were old enough to have received their 12-month vaccination. Four of the 17 cases were under four years old and therefore too young to have received their second scheduled measles-containing vaccine according to the National Immunization Programme schedule.
Only six of the 17 cases were diagnosed on their first contact with a health service (GP or ED). Three cases were diagnosed on their second visit; two cases on the third visit, one on the fourth, two on the fifth and one case on the sixth visit. The diagnosis of two cases was missed; they were diagnosed approximately five months later, during detailed assessment of ED triage notes to identify possible source cases. The median number of days from onset to notification was eight (range: three–178 days), the median number of days from rash developing to notification was four (range: zero–175 days).
The five index cases were between days four and six of illness when transmission occurred. None had been isolated within the health care facility. The seven secondary cases, established to have been infected in a health care setting, were present at the same time as their index case. Contact time ranged from 20 to 162 minutes. All secondary cases would have come within two metres of their index case while in the health setting. One secondary case was seen in the same treatment room as the index case and another case was standing near the index case in the registration line (Table 2). None of the five index cases and one of seven secondary cases had received at least one dose of measles-mumps-rubella (MMR) vaccine. Of the seven secondary cases, two were one year of age, one was 17 years old and four were between 30 and 39 years old.
* In South Western Sydney and Sydney local health districts.
Transmission of measles in healthcare settings may prove to be an important obstacle to the elimination of measles in developed countries like Australia. While Australia has high immunization coverage, there are a small proportion of those born between 1966 and 1981 (aged between 29 and 45 years) that may be susceptible because they were born after measles circulation began to decline but have not received two doses of measles vaccine. There are also occasional children who are susceptible because they are not vaccinated or vaccine has failed; fewer than 1% of people fail to develop immunity to measles following the second dose of vaccine.16 Young adults are highly mobile, have many social contacts and often have several visits to health care facilities before they are diagnosed. Many ED and GP waiting areas are large, have high throughput and waits can be long. These factors increase the probability of an acutely unwell and infectious measles case making contact with another susceptible person.
With limited public health resources, refinements to the national guidelines may be warranted. It will be essential to balance the role of health care facilities in the transmissions of measles with the high workload required by large numbers of contacts, many of whom are immune. The Australian measles guidelines defines waiting room contacts as “people who stayed in a waiting area at the same time as the case and people who waited in the waiting area or who were seen in the same consultation room up to two hours after the case left.”3 Two previous cluster investigations in 1981 and 1982 of transmission from a single case to contacts in a health facility indicated that airborne spread of measles can occur up to an hour after the index case has left the premises.17,18 However, even in the small outbreak reported here, non-isolated cases in health care waiting rooms often resulted in exposure to 100 or more individuals who needed to be traced to ascertain possible susceptibility to measles. Although our case series was small, all transmissions occurred to patients or relatives who were already in the health facility when the index case arrived or to patients or relatives who arrived while the index case was still in the facility. Hospitals and primary care facilities keep records of entry and exit times; in addition, some facilities keep records of the bed or treatment rooms occupied by the index case. Therefore, if resources are limited, focusing only on contacts who were present in a facility at the same time as the case may be warranted.
Delayed diagnosis has been indicated as a risk for transmission in many outbreaks in countries reaching measles elimination. The diagnosis of measles is difficult with early symptoms resembling many conditions. However, many doctors have never seen a case of measles and are unfamiliar with the more typical later features of rash, fever, cough and conjunctivitis. Continuing communication with GP and ED staff is vital to ensure that measles is considered as a possible diagnosis in persons with fever and rash, that appropriate tests are ordered and that the appropriate notification process is followed.
A review of nosocomial measles transmission identified health care workers as important sources of transmissions in health care facilities.9 In past outbreaks within Australia health care workers have been identified as secondary cases.1,4,8 While no health care worker was identified as a case during this outbreak, high rates of vaccination should be maintained in this group.
Measles cases in Australia have been mainly due to overseas acquired infections; however, this outbreak has shown continued transmission can occur within Australia in a small group of susceptible people. Exposure information collected during an outbreak is vital to ensure the source of infection can be determined, to identify sources of threats and to assist in developing prevention strategies. Currently, investigations focus on where the person travelled during their infectious period, thus allowing follow-up of contacts to prevent further transmission. While this is important, detailed information during the case exposure period is also important; knowing how transmission occurred can help inform prevention strategies, which become increasingly important when a country is close to elimination.
Many outbreaks in countries reaching elimination occur in children whose parents do not want their children vaccinated. This outbreak occurred in young adults, who were not vaccinated as a child or who did not know their vaccination status; no case was a conscientious objector. A high number of contacts with unknown vaccination status affected the efficiency of the investigation and may have resulted in unnecessary prescribing of normal human immunoglobulin. Past outbreaks have also demonstrated that verbal history of prior doses of MMR vaccine is unreliable.1
The information collected through this investigation was affected by recall bias: patients self-reported onset dates, date of rash appearance and activities during exposure and infectious periods. While onset and rash dates should be fairly accurate, it is possible that activities during exposure or the infectious period could have been left out or not accurately reported. This outbreak investigation relied on passive surveillance (i.e. for cases to be notified to the public health unit); therefore, cases could have been missed if they were not ill enough to seek medical care and if a doctor failed to diagnose measles.
In addition it was not possible to measure exact distance between the health care waiting room transmission cases and their index case; therefore, information from the health provider about room or bed allocation and entry and exist times was used to approximate distance and exposure time. Previous studies have shown that airborne transmission of measles is possible;17,18 however, no attempt was made to determine either the design and operation of air conditioning systems in these health care settings or their efficacy in limiting aerosol spread for this study.
As Australia moves towards measles elimination, follow-up of cases is important. In this small but well-documented series of secondary cases acquired in health care settings all were infected following direct, proximate contact of at least 20 minutes. A review of national guidelines should consider a more targeted follow-up to ensure a more efficient use of resources. Public health resources may be better spent on education of GP and ED staff to facilitate isolation on suspicion of measles and prompt diagnosis to reduce the possibility that infectious cases expose large numbers of people in these waiting room settings.
None declared.
None.