a Communicable Disease Control Department, Ministry of Health, Cambodia.
b Kampong Speu Provincial Health Department, Ministry of Health, Cambodia.
c World Health Organization, Phnom Penh, Cambodia.
d South Asia Field Epidemiology and Technology Network, Inc.
Correspondence to Maria Concepcion Roces (e-mail: rocesm@wpro.who.int).
To cite this article:
Vandy S et al. Vibrio parahaemolyticus enteritis outbreak following a wedding banquet in a rural village – Kampong Speu, Cambodia, April 2012. Western Pacific Surveillance and Response Journal, 2012, 3(4):25–28. doi:10.5365/wpsar.2012.3.4.004
Introduction: Foodborne outbreaks are common in Cambodia, but only a few investigations documenting the etiology and source have been conducted. In April, we learnt of 49 acute diarrhoea cases in a village following a wedding banquet. We undertook an investigation to identify the pathogen, source and mode of transmission.
Methods: We interviewed banquet hosts and food handlers to obtain the menu and guest list. Guests were asked about signs and symptoms and onset of illness, time of meal and food or drinks consumed. Rectal swabs were taken from 13 cases for culture. A case-control study was undertaken; cases were guests who had acute diarrhoea within three days after the wedding and controls were guests who remained well during the same time period.
Results: There were 256 guests. Of 69 interviewees, 52 got sick (attack rate 75%). Aside from diarrhoea, cases had abdominal pain (94%), vomiting (48%), nausea (42%) and fever (25%). Incubation periods ranged from seven to 51 hours (median 16.5). Rectal swabs from three cases grew Vibrio parahaemolyticus. Among the food and drinks served, vegetable salad with raw octopus was the only one associated with illness (odds ratio: 6.6, 95% confidence interval: 1.3–36.1, P = 0.01).
Discussion: Vegetable salad with raw octopus was the suspected vehicle for transmission of this Vibrio parahaemolyticus enteritis outbreak. Messages regarding the risks from eating raw seafood were disseminated, and food handlers were advised to cook seafood to high temperatures. Efforts to improve foodborne disease surveillance and food safety are being undertaken.
Vibrio parahaemolyticus is a gram-negative bacteria that inhabits marine environments and is a well known cause of foodborne disease outbreaks in south-eastern Asia.1 Vibrio parahaemolyticus infection is typically contracted by eating contaminated seafood such as raw or undercooked shellfish1,2 and was first identified as a cause of foodborne outbreaks in 1950 following an incident in Japan when 20 out of 272 ill persons died after eating sardines.3 In Taiwan, China it is believed that up to 71% of foodborne illness outbreaks from 1996 to 1999 were caused by Vibrio parahaemolyticus.4
In Cambodia, there is no routine reporting of food poisoning cases. However, an event-based surveillance system exists which captures reports from the media and includes a hotline number that health workers or the general public can call to report suspected outbreaks. These reports are then investigated by Rapid Response Teams (RRTs) as needed.
On 10 April 2012, the Kampong Speu Provincial RRT informed the Communicable Disease Control Department of 49 cases with acute diarrhoea seen at the Veal Angpopel Health Center during the past two days after most of the cases attended a wedding party on 8 April held in Tbaung Boeung village. Upon receipt of the report, a RRT travelled to the village, located about one and a half hours from Phnom Penh by car, to conduct an outbreak investigation. The objectives of the investigation were to identify the etiologic agent, source and mode of transmission and to recommend appropriate public health measures.
This paper details the clinical, laboratory and epidemiological findings from this outbreak investigation and is the first documented Vibrio parahaemolyticus enteritis outbreak from Cambodia in the English literature.
We interviewed key informants (health centre staff, hosts of the wedding party, some persons involved in food preparation and a few patients). A list of party attendees and the menu were obtained. Wedding attendees came from eight provinces, and at the time of the field investigation many attendees had returned to their home provinces. We were therefore only able to interview attendees who lived in the village where the wedding was held and a nearby village. A team of eight persons interviewed these wedding party attendees in person using a standard foodborne illness questionnaire. Data on demographic information, signs and symptoms, onset of illness, time of meal and food items consumed during the party were obtained.
Since we were only able to interview 27% of the guests (69/256), we used a case-control study design. Cases were wedding party attendees who developed acute diarrhoea (> three loose bowel movements in a day) after the party anytime from 8 to 10 April. Controls were wedding party attendees who remained well during the three days after the party.
We obtained rectal swabs from 13 cases who agreed to have samples taken from them. The samples were sent to the laboratory at the National Institute for Public Health, Cambodia for bacterial culture.
Data were entered into a computer and analysed using Epi Info. We calculated odds ratios, confidence intervals and P values using the Fischer's exact test (2-tailed) and Yates corrected chi-squared test.
The wedding party was held on 8 April from morning until evening at the bride’s family home and was attended by 256 guests. Food was served from 15:00 to 19:00. The menu consisted of the following: vegetable salad with raw octopus, chicken soup with coconut milk, pork salad, fried fish with sauce, chicken soup with lime and rice. Beverages served were beer, soft drinks and water. Guests could request to have ice with their drinks.
The various food items were prepared by a team of 20 people. Food preparation began early in the morning, and some dishes (soups and fish) were reheated during the day. The main ingredients for the vegetable salad (carrots, lettuce, various herbs, garlic, peanuts, bean sprouts and octopus) were chopped and kept in separate bowls on a long table. During meal time, a server would mix the various ingredients in a serving plate and place the plate on the guests’ tables.
Since there were no left-over food samples, none was available for laboratory testing.
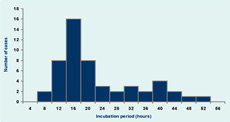
Of 69 guests interviewed, 52 got sick (attack rate 75%). The majority (46/52 or 88%) of the cases had watery diarrhoea, five (10%) had mucoid stools, while one (2%) had bloody diarrhoea. Other signs and symptoms of cases were abdominal pain (94%), vomiting (48%), nausea (42%) and fever (25%). Eighteen cases were hospitalized. All cases recovered (Figure 1).
Of the 13 rectal swabs collected, three were positive for Vibrio parahaemolyticus. All other specimens had no enteropathogenic organisms isolated. Subtyping of the Vibrio parahaemolyticus isolates was not done.
The incubation periods of the cases ranged from seven to 51 hours with a median of 16.5 hours.
Fifty-two cases and 17 controls were included in the study. The age and gender distribution of cases and controls were similar. Fifty-four per cent of cases and 53% of controls were male. The median age for cases was 40 years (range 10–75) and 37 years for controls (range 5–63).
Among the food items served, only the vegetable salad with raw octopus was found to have a statistically significant association with illness with an odds ratio of 6.6 (95% CI: 1.3–36.1) (Table 1). Several interviewers reported that non-wedding party attendees developed diarrhoea after eating vegetable salad taken home by wedding party guests and that rectal swabs from two non-guests were also positive for Vibrio parahaemolyticus.
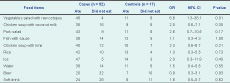
OR – odds ratio; CI – confidence interval.
Through interview with those involved in the food preparation, it was revealed that the octopus from the vegetable salad was bought from a market (30 minutes travel time). Seafood sold in this market comes from a southern coastal province. From source to market, the seafood is transported in ice boxes (2.5 hours travel time) and kept in ice at the market. However, when the octopus was bought from the market, it was packed in a plastic bag without ice.
The RRT educated the food handlers about proper food handling, preparation and hygiene. The following messages were provided to the food handlers in this outbreak:
This foodborne outbreak was most likely caused by Vibrio parahaemolyticus from contaminated raw octopus served at the wedding. Both the signs and symptoms and incubation periods of the cases were compatible with Vibrio parahaemolyticus enteritis,2 and Vibrio parahaemolyticus was also isolated from rectal swabs of cases.
The epidemic curve was that of a common point source outbreak and the case-control study suggested that the vegetable salad with raw octopus was probably the vehicle for transmission in this food poisoning outbreak. Despite the limited sample size, particularly the small number of controls, there is convincing evidence that the vegetable salad with octopus was the vehicle for transmission. This includes the anecdotal finding of Vibrio parahaemolyticus-positive cases among family members that did not attend the wedding party but ate the vegetable salad brought home by household members who attended the party. Among the food items served during the wedding party, only the vegetable salad was brought home by the guests since this was a special dish and easy to pack.
Among the ingredients in the salad, the raw octopus most likely contained the bacteria. Vibrio parahaemolyticus infection from undercooked shellfish and bivalves, particularly oysters, is well described in the medical literature.1,2,5 This study provides evidence for contamination of saltwater octopus with Vibrio parahaemolyticus. Saltwater octopus is a food item commonly consumed in Cambodia.
As this study emphasizes the dangers of consuming raw seafood in Cambodia, an important issue raised by this investigation is the need to improve food safety. Public health messages on the importance of cooking sea food well before consumption, especially during special occasions when large numbers of persons can become acutely infected, were one such measure employed by the RRT in this investigation.
Foodborne outbreak surveillance in Cambodia is conducted principally through an event-based surveillance system. Mechanisms for reporting and investigating large foodborne outbreaks with laboratory confirmation should be considered to better understand the most frequent causes of such outbreaks in the country. The existing indicator-based surveillance system could be used to detect clusters of diarrhoea disease, thereby triggering an outbreak investigation with sample collection.
Finally, this study demonstrates the importance of including questions about raw seafood in salads and vegetable dishes during investigations of foodborne outbreaks.
None declared.
None.
We are grateful for the cooperation and support of the local health staff and village residents during the field investigation. We also thank the laboratory staff of the National Institute of Public Health, Cambodia for testing the clinical samples obtained from some cases.