a Lianyungang Municipal Center for Disease Control and Prevention, Lianyungang, Jiangsu Province, China.
b China Field Epidemiology Training Programme, Beijing, China.
c Jinan Municipal Center for Disease Control and Prevention, Jinan, Shandong Province, China.
d Ganyu County Center for Disease Control and Prevention, Ganyu, Jiangsu Province, China.
e Jiangsu Province Center for Disease Control and Prevention, Jiangsu Province, China.
Correspondence to Zhang Ting-lu (e-mail: tlzhang66@gmail.com).
To cite this article:
Zhang TL et al. Investigation of an outbreak of cutaneous anthrax in Banlu village, Lianyungang, China, 2012. Western Pacific Surveillance and Response Journal, 2012, 3(4):12–15. doi:10.5365/wpsar.2012.3.4.005
Objective: After notification of a suspected case of anthrax following the slaughtering of a sick cow in Banlu village, an area that has not had any anthrax cases for decades, we aimed to confirm the outbreak, determine the transmission mechanism and implement control measures.
Methods: The outbreak response team interviewed all people that had contact with the sick cow. Three types of cases’ specimens were collected and tested by blood smear, real-time polymerase chain reaction (PCR) and the gold colloid method. Traceback of potentially contaminated meat and cattle were conducted.
Results: There were five confirmed and three probable cases verified among 17 people who had contact with the sick cow – an attack rate of 47%. The incubation period ranged from one to eight days with a median of two days. All eight cases had lesions. All were native residents of Banlu village aged between 21 and 48 years. Five male cases were professional butchers; two females and one male were temporary assistants. The sick cow’s meat and hide, as well as all cattle processed at the same time, were recalled. Hypochlorite was used to disinfect the contaminated environments, butchering facilities and the contacts’ personal effects.
Conclusion: This outbreak was caused by anthrax bacillus transmitted to contacts from the tissues of the sick cow. Control of the outbreak was managed by recalling all potentially infected meat and disinfecting the slaughter house and the suspected cases’ personal effects and environment.
Cutaenous anthrax often occurs among herdsmen or butchers in pasture areas in the northern or western parts of China each year1,2 and in many developing countries like India and Bangladesh.3,4 In Lianyungang, a coastal prefecture in the eastern part of China, the major crops are wheat and rice, although thousands of cattle are imported for slaughter from pastures in the northern part of China each year. Banlu village, located in the north of Lianyungang prefecture with a population of 1466 in 367 households, has a long history of slaughtering cattle. There has been no cutaenous anthrax cases reported in Lianyungang prefecture in past decades.
On 2 August 2012, the Lianyungang Centre for Disease Control (CDC) was notified from a hospital doctor of a case of anthrax with three lesions on both of his hands (two lesions on his left little finger and another one on the back of his right hand) after slaughtering a sick cow in Banlu village. This case worked at the largest of the three slaughter houses in the village. After confirming the information by telephone, several epidemiologists and laboratory staff from the CDC were sent to the village for further investigation the same day. Information about this suspected case of cutaneous anthrax was also sent to the veterinary officers. We describe the outbreak investigation that followed.
According to national guidelines,5 we conducted face-to-face interviews with all suspected cases defined as slaughter house workers who were exposed to the tissues of the sick cow. This included anyone involved in the slaughtering, skinning, cutting and/or washing of meat and viscera/organs and/or selling the meat of the sick cow. The outbreak case definitions were then defined as: a probable case had skin lesions involving vesicular eruption and/or black eschar; a confirmed case was a probable case with one of three laboratory-positive results: the anthrax bacillus was detected by blood smear; serum, liquid from blisters or eschars tested positive by real-time polymerase chain reaction (PCR); or the anthrax antigen tested positive by the gold colloid method.
Information involving name, age, occupation, work practices, disease onset, symptoms and treatments were recorded on questionnaires. We also collected information from the medical records from village clinics and hospitals. Excel 2003 was used for the database, and data were analysed with Epi Info 3.5.1. Three types of clinical specimens were collected: blood, eschar and blister fluid. The blood smear with Gram staining was done at the Lianyungang CDC Laboratory and the PCR and the gold colloid method were done at Jiangsu Province CDC Laboratory. On 2 August 2012, the veterinary officers arrived at Banlu village for the traceback investigation and the recall of potentially contaminated meat and cattle with the outcome reported to the outbreak investigation team. Ethics approval was not required as this was an outbreak investigation, although patient consent was obtained before taking specimens.
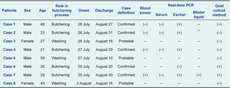
Among the 17 suspected cases (seven butchers, five temporary assistants who washed the meat and organs of the sick cow, four vendors and one person who purchased the hides), eight met the outbreak case definitions: five confirmed and three probable cases (Table 1). The attack rate was 47.1% (8/17). There were six male and two female cases aged between 21 and 48 years old, with a median age of 28 years. Five male cases were professional butchers; two female cases and one male case were temporary assistants. All eight cases were native residents of Banlu village; Case 1 was the father of Case 2; Case 8 was the mother of Case 4.
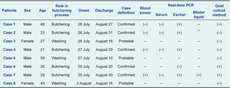
PCR – polymerase chain reaction; (+) – positive; and (–) – negative.
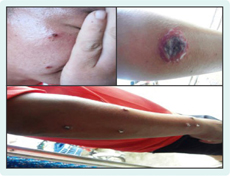
All eight cases had lesions, fever, dizziness, headache, cough, chest pain, fatigue and armpit lymphadenectasis or submaxillary lymph node intumescence; 50% had a fever over 39°C after onset of disease. The highest number of lesions in a single case was nine; the largest lesion was 3.5 cm in diameter, and the smallest was 0.2 cm in diameter (Figure 1). With regards to lesion location, 41% (9/22) were on arms, 27% (6/22) on legs, 23% (5/22) on hands and 9.1% (2/22) on faces.
The sick cow was slaughtered on 25 July 2012. Three cases had disease onset the next day, two cases on 27 July, one case on 29 July, one case on 30 July and the final case on 2 August. The incubation period ranged from one to eight days with a median of two days (Figure 2). On 4 August 2012, the eight cases were sent to a Lianyungang communicable disease hospital for isolation and treatment. Patients were discharge when the eschar responded to treatment and sloughed off. With penicillin treatment, three probable cases and five confirmed cases were cured and discharged before 1 September (Table 1).

Of the five confirmed cases, three were confirmed by PCR from eschar specimens (Case 1, Case 2 and Case 4), one by gold colloid method from a blood specimen (Case 6) and one (Case 7) by blood smear, PCR and gold colloid method (Table 1).
The sick cow was manually butchered on 25 July because one of its legs had broken during the travelling period. The traceback investigation found that 200 cattle were transported to the slaughter house from a pasture in the northern part of China on 25 July. On 7 August, hundreds of kilograms of meat and hide from the sick cow were recalled (Figure 2).
Twenty-six cattle were butchered by an automated process in the slaughter house; this meat was destroyed by police on the road to Shanghai. Thirty-four cattle were sold to Nanjing, and the meat was destroyed by the Nanjing local government. A further 43 cattle were still in Banlu village waiting for butchering and these were euthanized and buried in a deep pit by the Jiangsu Province Food and Drug Administration on 11 August. Another 90 cattle were sold to a neighbouring province, and no further intervention information by that local government was provided.
As the slaughter house sewerage and butchering site had been contaminated by the sick cow’s blood, wastewater and excreta, the contaminated environments, butchering facilities and the contacts’ personal effects were disinfected. Hypochlorite was used to disinfect the slaughtering site, butchering facilities and the suspected cases’ personal effects every day from 2 to 18 August 2012. The medical trash and the wards in the clinic/hospital were disinfected every day until 31 August 2012.
We report on an outbreak of cutaneous anthrax that occurred in Banlu village, Lianyungang between 25 July and 14 August 2012. All cases had an incubation period of one to eight days, consistent with cutaneous anthrax,6 and five cases tested positive were confirmed by laboratory testing. The mode of human transmission was through contact with the tissues of the sick cow thought to be infected by anthrax bacillus in its native pasture. The slaughter house had purchased 200 cattle with valid veterinary quarantine certificates from a pasture in the northern part of China in July 2012 where cutaenous anthrax has been reported before.7 In an outbreak in 2005, all cases were involved in the butchering of sick or dead cows six days before onset of disease.7
Similar outbreaks have been recently reported in India3 and Bangladesh.4 In West Bengal in India an outbreak of cutaneous anthrax occurred following the slaughter of a dead bullock in a small tribal village. Most cases (81.8%) were exposed to the bacteria during butchering, although the attack rate of 7% was much lower than that in Banlu village.3 In Bangladesh, 15 cutaneous anthrax cases were reported between April and August 2011, which also occurred after slaughtering with symptoms similar to those in this outbreak.4
The control measures used in this outbreak included the recall of all potentially infected meat and hides from the cattle at the slaughter house at the same time the ill cow was processed. Disinfection of both the slaughter house and the suspected cases’ personal effects and environment was also done. As the investigation occurred nine days after exposure, and the slaughter house is routinely hosed out, we did not test any environmental samples for the presence of anthrax.
Our recommendations from this outbreak investigation include establishing surveillance in Banlu village for anthrax, educating butchers on the modes of anthrax transmission and care of skin abrasions, establishing prevention methods including personal cleanliness and refraining from purchasing or killing dead or dying cattle and other animals.
None declared.
None.