a Viet Nam Field Epidemiology Training Programme.
b General Department of Preventive Medicine, Ministry of Health, Viet Nam.
c World Health Organization Representative Office, Hanoi, Viet Nam.
Correspondence to Phan Thanh Tinh (e-mail: mdtinh@gmail.com).
To cite this article:
Tinh PT et al. Epidemiological and clinical characteristics of patients who died from Influenza A(H1N1)pdm09 in Viet Nam. Western Pacific Surveillance and Response Journal, 2012, 3(1):6-11. doi:10.5365/wpsar.2011.2.3.003
We describe the epidemiological and clinical characteristics of patients who died from influenza A(H1N1)pdm09 in hospitals in Viet Nam between August 2009 and March 2010.
Of 58 fatal cases, 32 (55%) were below 30 years of age and 14 (24%) were pregnant females. Forty-five (78%) patients had at least one underlying medical condition including chronic heart, kidney or lung diseases or pregnancy. Twelve (21%) cases sought medical attention on the day of symptom onset. Only 13 (36%) of 36 cases for whom treatment data were available had been given antiviral drugs within the recommended two days of symptom onset.
The clinical and epidemiologic characteristics of the patients who died from influenza A(H1N1)pdm09 are similar to those reported from other countries. To improve preparedness and response to future pandemics, Viet Nam needs to strengthen the surveillance of influenza; increase laboratory capacity to test for influenza viruses; and develop strategies for promoting the timely attendance of at-risk individuals at health facilities and the early administration of antiviral drugs, particularly for persons with underlying medical conditions and pregnant females.
The emergence and spread of A(H1N1)pdm09 was first reported in Mexico in the spring of 2009.1 This novel virus then spread rapidly across the world. On 11 June 2009, the World Health Organization (WHO) declared this event the first influenza pandemic of the 21st century. By March 2010, 213 countries had reported cases with laboratory-confirmed A(H1N1) pdm09 and 17 483 associated deaths.2,3
The pandemic was introduced into Viet Nam via Ho Chi Minh City in early June 2009 by passengers flying in from countries affected by the pandemic, particularly the United States of America and Australia. The number of cases increased in August as the virus spread to other regions, and by March 2010, 11 208 laboratory-confirmed cases were reported across Viet Nam. To strengthen Viet Nam’s preparedness, surveillance and response capacities, we conducted a retrospective study of the epidemiological and clinical features of patients who died from A(H1N1) pdm09 to determine the frequency of underlying medical conditions and the use of antiviral drugs by health staff.
The definition of a suspected case with A(H1N1) pdm09 was the sudden onset of fever (>38°C) plus symptoms of an acute respiratory infection that started within a week of travel to an affected area or history of close contact with a patient who had laboratoryconfirmed A(H1N1)pdm09. Confirmed influenza A(H1N1)pdm09 was defined as a suspected case who tested positive on real-time RT–PCR assay in accordance with the protocol from the US Centers for Disease Control and Prevention.4 Between August 2009 and March 2010, a A(H1N1)pdm09 related death was defined as death in a person who had laboratory confirmed A(H1N1)pdm09, regardless of the underlying cause of death. We selected this study period because the first known death from influenza was in August 2009, and we continued the enhanced hospital-based surveillance for deaths until March 2010.
In response to the pandemic, a system was established to enhance surveillance across Viet Nam. All hospitals in Viet Nam were requested to collect naso-pharyngeal swabs from all patients who had an acute respiratory infection. The swabs were sent initially to the four reference laboratories accredited by the Ministry of Health, namely, the laboratories at the National Institute of Hygiene and Epidemiology in Hanoi, the Ho Chi Minh City Pasteur Institute, the Nha Trang Pasteur Institute and the Tay Nguyen Institute of Hygiene and Epidemiology in Buon Me Thuot. However, as the number of cases rose rapidly by October 2009, the Ministry of Health authorized laboratories at 16 tertiary level hospitals with adequate facilities, equipment, appropriately trained staff and standard operating procedures to conduct the confirmatory RT–PCR testing. Furthermore, from the first week of October 2009 onward, testing was limited to persons at risk of severe complications (pregnant females, persons with chronic diseases and young children), and to patients with severe respiratory illness (labelled as restricted laboratory testing in Figure 1).
Hospitals reported any deaths among patients with laboratory-confirmed A(H1N1)pdm09 on a standard form to the provincial preventive medicine centres; the latter forwarded the reports to the respective regional Institutes of Hygiene and Epidemiology or Department of ommunicable Disease Control, Ministry of Health, in Hanoi. The data included identifying and demographic information, date of onset of symptoms and of the first attendance for health care, presence of underlying medical conditions and pregnancy, details of antiviral administration, date and place of death, medical examiner reports and the death certificate.
The denominator for calculating the mortality rate was based on Viet Nam’s 2009 population census, i.e. a total population of 85.8 million.
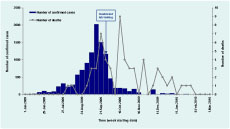
The first death in a person with laboratoryconfirmed A(H1N1)pdm09 was reported in August 2009 in the central province of Khanh Hoa, and by March 2010 a total of 58 deaths had been reported. The overall mortality was 0.7 per million population.
The number of deaths increased gradually in August 2009 to peak in late September 2009, in parallel with the number of notified laboratory-confirmed Pasteur Institutes that in turn submitted them to the cases, but dropped sharply over the following three weeks (Figure 1). The drop in number of deaths coincided with the drop in the number of laboratory confirmed cases, and this occurred one week before the Ministry of Health recommended it was no longer necessary to test everyone with symptoms of an acute respiratory illness. The number of deaths then increased sharply to reach the second peak in late October 2009 and early November 2009.
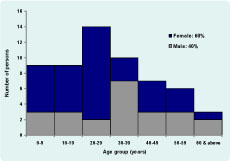
The age range of the 58 persons who died was between 10 months and 64 years, with a median of 29 years. There were 32 (55%) deaths in patients below 30 years of age, 49 (84%) deaths below 50 years of age, and seven deaths (12%) in children less than five years of age. Females accounted for 35 (60%) of the deaths (Figure 2).
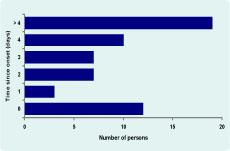
Twelve (21%) of the 58 patients who died sought health care on the day the symptoms first appeared (Figure 3); eight of them had underlying conditions, and four females were pregnant, one of whom also had asthma. A further 10 (17%) patients attended within one to two days, seven (12%) attended on day three after symptom onset, 10 (17%) on day four and the remaining 19 (33%) attended more than four days after symptom onset.
The first place of attendance for health care was as follows: two (4%) at commune-level and private health care clinics, 18 (31%) at a district or municipal level hospital, 28 (48%) at a provincial level hospital and 10 (17%) at a tertiary level hospital.
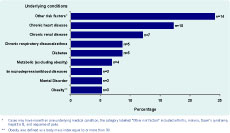
Of the 58 persons who died, 45 (78%) had at least one underlying medical condition (Figure 4). An underlying medical condition was reported in nine of 10 cases (90%) aged over 50 years, in 24 of 30 cases (80%) aged between 20 and 49 years and in 12 of 18 cases (67%) aged below 20 years. The mean interval between onset of symptoms and death in these patients with underlying medical conditions was 10 days while in the remaining 13 cases the interval was 12 days.
Data on the use of antiviral treatment (oseltamivir) was available on 36 (62%) of the 58 cases. Of these, only 13 (36%) had received medical care within two-days of symptom onset and received the drug within this period as recommended by WHO.5 Treatment data on the other nine cases who received medical care in this period was not available. The remaining 23 cases received treatment after this period, while treatment data on the other 13 cases who sought care more than two days after symptom onset was not available.
Thirty-three (55%) of 58 cases required mechanical ventilation; the median interval between symptom onset and start of ventilation was five days.
Of the 35 females who died, 14 (40%) were pregnant, and their ages ranged from 15 to 39 years, with a median of 24 years; eight (57%) of the 14 pregnant females had an additional underlying medical condition, including heart disease, kidney disease, chronic lung disease and other metabolic disorders. Ten females (71%) were in the third trimester of pregnancy and the remaining four (29%) were in he second trimester.
Between August 2009 and March 2010, 58 persons were reported to have died from laboratory-confirmed A(H1N1)pdm09 in Viet Nam, yielding an overall mortality of 0.7 per million population. Most patients were young or middle-aged, and had an underlying medical condition or were pregnant. Only 13 of 22 patients who were treated within the first two days of symptom onset were given oseltamivir within the recommended two days after onset of symptoms; this included six of the seven pregnant females who sought care within two days of symptom onset.
The overall A(H1N1)pdm09 mortality in Viet Nam is low when compared with reports ranging between 2.2 and 3.3 deaths per million in northern hemisphere countries, except in Japan, where the mortality rate was 0.2 per million.6 The most likely explanation for the low mortality in our study, as elaborated under ‘limitations’ below, is an underascertainment of the number of deaths.
Of the 58 deaths, 49 (84%) were aged below 50 years, and just over half (55%) were below 30 years. Consistent with other reports,6–9 deaths in this younger age group contrasts with the experience from seasonal influenza in the United States of America where about 90% of deaths are in those aged over 65 years.10 This observation probably reflects an age-cohort effect as the elderly were probably protected from severe disease due to previous exposure to antigenically similar viral strains.11
Of all deaths, 45 (78%) had an underlying medical condition. This finding is also similar to the experience in other countries. In The United Kingdom and Greece, for example 72% and 82% of the deaths attributed to A(H1N1)pdm09, respectively, had at least one underlying risk factor.8,9 In France, over half the patients had an underlying risk factor, including obesity, although obesity is usually not considered a risk factor for deaths from seasonal influenza.7 However, it is possible we may have overestimated the frequency of an underlying medical condition in our study because from October 2009 onwards, laboratory confirmation of influenza was selectively recommended only in people with an underlying medical condition or with severe disease.
Fourteen (40%) of the 35 females who died were pregnant. The United Kingdom,8 but not Greece,9 reported pregnancy as a risk factor for dying. A study in the United States also revealed pregnancy as a risk factor for dying, but showed that antiviral treatment within two days of onset of symptoms reduced this risk compared with treatment after four days of onset of symptoms.12
Although the trend in the number of reported deaths mirrored the rising incidence of confirmed cases from late August to late September, we were unable to explain the sharp drop in deaths through mid-October. It is possible that health staff may not have been collecting specimens for laboratory testing from all cases with severe disease who died up to this period. Interestingly, the number of cases reported with confirmed influenza also started dropping at the same time and before laboratory testing of all cases was stopped as the disease started spreading rapidly across the country. Possible explanations for the drop in the number of confirmed cases include: fewer persons seeking health care once the relatively mild nature of the disease was apparent and inability of the laboratories to maintain a surge capacity to test all specimens. The sharp rise in deaths in late October to early November 2009 probably reflects the priority accorded to testing a larger proportion of patients at high risk of severe complications such as pregnant females, persons with chronic diseases, young children and patients with severe illness.
The major limitation of this study is the likely underascertainment of the number of deaths across Viet Nam, but this assumption was not evaluated formally. Possible explanations for this may include lack of reporting of deaths that may have been due to influenza but were not tested for influenza and failure to test all patients with severe disease who died subsequently (post-mortem examinations of unexplained deaths were not conducted). An additional limitation was that we did not have data on whether nine of 22 patients who attended within two days of symptom onset had received anti-viral treatment, thus precluding further analysis on whether health staff provided timely treatment with antiviral drugs.
In conclusion, our findings on the clinical and epidemiologic characteristics of people who died from A(H1N1)pdm09 are similar to those in other countries. The key lesson for Viet Nam is the need to strengthen the surveillance of influenza in the context of addressing the multiple challenges for strengthening surveillance and control of all the communicable diseases, particularly those with epidemic potential. It is relatively simple to recommend from our study that Viet Nam must develop and fund strategies to strengthen surveillance of influenza-like illness, promote early health care attendance of at-risk individuals with influenza and offer timely antiviral treatments. In recent years, Viet Nam has been developing and implementing a range of strategies to address these challenges in collaboration with its national experts and international partners.
None declared.
None.