a Hunter New England Population Health, New South Wales, Australia.
b School of Public Health, James Cook University, Queensland, Australia.
c University of Newcastle, New South Wales, Australia.
d Hunter New England Health, New South Wales, Australia.
Correspondence to Keith Eastwood (e-mail: keith.eastwood@hnehealth.nsw.gov.au).
To cite this article:
Eastwood K et al. Field exercises are useful for improving public health emergency responses. Western Pacific Surveillance and Response Journal, 2010, 1(1):12-18. doi:10.5365/wpsar.2010.1.1.003
Problem: Emergencies resulting from disease outbreaks and extreme environmental events present significant challenges for health services.
Context: Preparing to effectively manage emergencies is a core activity in public health units. Field exercises support consolidation of biopreparedness by testing plans, identifying weaknesses, providing training opportunities and developing surge capacity.
Action: An extended field exercise to test response to a novel influenza strain was conducted in New South Wales, Australia in September 2008, eight months before the influenza A(H1N1) 2009 pandemic emerged. Lasting four days and involving over 300 participants, the exercise was set in the early response phase with the staggered presentation of 41 cases to 36 emergency departments in the health area. An additional 150 contacts were written into a complex scenario to test the public health response.
Outcome: The subsequent pandemic emergence in mid-2009 offered a unique opportunity to assess the field exercise format for disaster preparedness. Most roles were adequately tested with recognized benefit during the actual pandemic response. However, the exercise did not adequately challenge the public health planning team that synthesizes surveillance data and forecasts risk, nor did it identify planning issues that became evident during the subsequent pandemic.
Discussion: Field exercises offer the opportunity to rigorously test public health emergency preparedness but can be expensive and labour-intensive.
Health emergencies such as large communicable disease outbreaks and severe environmental events often require lengthy responses and a sustained work effort across the health sector. Maintaining a heightened response over weeks or months presents a major challenge for which many health services are ill prepared. One likely scenario is the emergence of a novel infectious disease agent, for example an antigenic shift that results in a pandemic influenza strain. These occur on average every 20–30 years, placing a major burden on health services and society due to the increased morbidity and mortality.1
Early in a pandemic, public health activities aim to delay transmission using various containment measures including: identifying and isolating cases and contacts; encouraging household infection control; adopting social distancing measures; providing health advice; and using antiviral medication. Exercises improve preparedness by testing plans and systems under controlled conditions, increase local awareness and provide training opportunities.
The Commonwealth government provides overarching policy and direction to the eight Australian states and territories; at the state/territory level there is further subdivision into regional health services that are responsible for community response and individual care. Like many federated countries, Australia’s three layers of governance potentially complicate communications during health emergencies.2 Australia has invested in pandemic planning and exercises at a national and state level to test border control, inter- and intra-government decision-making, deployment of the National Medical Stockpile, national health emergency response and public communications,3,4 but extended exercises at a regional level are uncommon.
On 7 May 2009, just eight months after the conclusion of our field exercise, the first case of pandemic influenza was detected in Australia.5 The Commonwealth government instituted aggressive containment measures to reduce disease transmission according to the national plan.6 Cases and contacts were requested to stay in home isolation/quarantine for up to seven days and take antiviral medication, as had been practised during the exercise. This placed us in a unique situation to assess the effectiveness of our field exercise in preparing for an actual pandemic event.
A regional New South Wales (NSW) health service conducted a four-day field exercise to simulate the range, complexity and work intensity during the early response to a large disease outbreak. Many exercises use virtual or desktop formats, but given the relatively large geographic area with a dispersed population, 36 Emergency Departments (EDs) and the varied resource capacity across the area, a field exercise was chosen to ensure participants and plans were suitably challenged. Public health staff and surge staff completed activities in exactly the same way expected of them in a true health emergency. The exercise control team regulated the ‘injects’ but allowed the scenario to flow naturally using actors trained to provide plausible input. Independent facilitators ensured the exercise was kept within pre-determined guidelines and avoided risk to players and the public.
The Hunter New England Health Research Ethics and Governance Unit did not require ethics approval since the study was regarded as a training exercise.
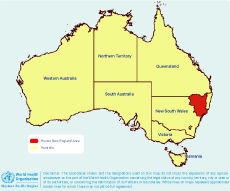
The exercise was conducted from 21 to 24 September 2008 in the Hunter New England Health Area, a region covering 130 000 km2 (Figure 1).
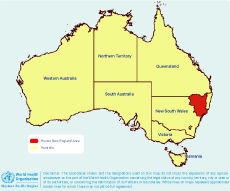
The population of approximately 865 000 is concentrated on the eastern coastline, with public health offices located in Newcastle, Tamworth and Taree (Figure 2). The area also includes large inland towns and remote outback Aboriginal communities as far as 500 km from the coast.7

The scenario was designed by an independent team over a period of six months with the support of a part-time project officer. Twenty external facilitators and umpires provided input through teleconferences held before the exercise. Surge staff, actors and public health personnel provided their time without charge against the exercise cost centre.
The exercise included:
A full Incident Command System (ICS) hierarchy was activated from the emergency operations centre. ICS staff included an incident controller and operations, planning, logistics and finance teams. Surge staff were recruited before the exercise, including 60 operations personnel. The operations team consisted of five separately located units of four people (an experienced team leader and three new nurses in each shift). Daily situation reports were prepared by the public health planning team and distributed to response personnel.
There were other significant exercise features.
The umpires and facilitators used a structured evaluation sheet to record their observations. They received training before the exercise began and provided comments on four areas: teamwork, communications, documents/materials and decision-making.9 At the conclusion of each day’s activities, structured debriefings were conducted with all players, to record aspects that worked well and identify weaknesses in plans and operations.10
The following shortcomings were identified during the exercise evaluation with most being addressed in a revised disaster plan before emergence of the 2009 influenza pandemic.
During the early response to the 2009 pandemic (the Containment Phase), the disaster response team was activated using our updated regional disaster plan and revised ICS public health staffing structure. The operations and logistics teams principally comprised public health and surge staff who had been involved in the field exercise. The efficiency of emergency operations centre telecommunications, videoconferencing and information technology services and the functions of the operations team were considerably enhanced by prior exercising.11
In contrast, it soon became evident that the public health planning team was under-resourced and unable to adequately meet requests from the operations team. Additional statistical assistance, not previously identified during the exercise, was needed to prepare a range of reports (worklists and quality checks) from the NetEpi database to assist the operations team with their duties.
Post-pandemic debriefs identified the need for the planning team to monitor the ‘epidemiological story’ by conducting a more systematic review of information collected during interviews, media reports and traditional surveillance data. The ICS framework was revised to include all planning functions within the structure (Figure 3).

Responding to a large infectious disease outbreak differs markedly from the management of disasters like an aeroplane crash which usually have an acute presentation but rapid resolution.12 A large disease outbreak involves a protracted response and warrants extensive preparation. Our field exercise provided an excellent training opportunity for the 2009 influenza pandemic and allowed prior testing and revision of local plans. It was particularly valuable in identifying and preparing surge operational staff.
Identifying surge capacity may be problematic for some health services. We employed clinical nurse consultants from non-acute areas such as the sexual health unit and stomal therapy and found them to have excellent skills. Data managers and statisticians were seconded from the area’s performance planning unit and readily adapted to their roles. Three Master of Applied Epidemiology graduates (from the Commonwealth’s field epidemiology training programme) and a National Centre of Epidemiology and Population Health lecturer were principal contributors to the exercise and other graduates were involved to a lesser extent. This programme provides surge response to public health emergencies in Australia and the Region but is currently under threat of closure.
There are few detailed published reports of pandemic exercises, although parallels can be drawn from bioterrorism drills.12,13 It appears that field exercises are only rarely deployed due to cost and resource implications,12 but they often identify fundamental issues that are unlikely to be recognized using desktop exercises.4,14,15
The pandemic response highlighted unresolved planning issues that had either not been identified during the exercise, or were inadequately addressed.
Our observations suggest that the full range of public health planning duties is poorly understood and this is likely to be reflected in preparedness, an observation recognized by others.14 We interpret this role to include the following:
Many of these priorities did not fully emerge during the field exercise possibly because the case-load and relatively short period of four days were insufficient to reveal these deficiencies. It was only during the extended pandemic response and when the database became larger and more complex that these became evident. Thus, while the field exercise provided an adequate opportunity for testing case and contact management it did not go far enough in meeting planning team needs. This could have been addressed through providing more hypothetical cases and contacts in the exercise database, or possibly telescoping the pandemic scenario’s time-frame. Investment in testing the role of planning is important and may be best achieved through realistic desktop exercising, perhaps nested within a field exercise.
An extended and realistic pandemic field exercise provided major benefits in preparing for the actual 2009 pandemic response and for generic public health disaster planning. It was particularly suited for the operations team in testing surge capacity. The principal exercise weakness was that it failed to adequately challenge the public health planning team. Our experiences indicate the importance of clarifying the scope of planning in disaster response, identifying the expertise required for the team and providing them appropriate exercise and training opportunities.
None declared.
Hunter New England Health Service provided funding for a part-time project officer for
Conducting a large field exercise requires immense cooperation across the breadth of the Hunter New England Health Service including the Area Executive Team, Emergency Departments, Referral and Information Centre, Infection Control Unit, Disaster Unit, the area Operations Centre and Clinical Nurse Consultants who were involved as surge staff. The Population Health Unit was outstanding and involved the Planning, Operations and Logistics Teams, Administration, Health Promotion, Indigenous staff and the CATI Team. We are particularly grateful for our colleagues who acted as evaluators, facilitators and technical advisers: Derene Andersen, Paul Armstrong, Paul Bibo, Philippa Binns,
Lessons for planning
Conclusion
Conflicts of interest
Funding
six months. None of the authors were paid for involvement in or attendance at the field exercise.
Acknowledgements
Tony Byrnes, David Coleman, Kevin Cooper, Peter Davidson, Debra El Saadi,
Ulrich Erlinger, Marianne Gaul, Simon Gould, Catherine Hugo, Paul Kelly, Helen Kendall, Gosta Liljeqvist, Desiree O’Brien, Rhonda Owen, Neil Parker, Glenn Pearce, Scott Pearce, April Roberts-Witteveen Eleanor Sullivan, Chabela Torres and Catherine Turner.
Christine Fraser and Sheryn Sommerville provided excellent project support. Thanks to
Lutz Ehlkes for assistance with the graphics.
References:
Publications/WHO+Influenza+Pandemic+Preparedness+Checklist.pdf [accessed
22 October 2010].
E4580DA8A091F993CA25781E000F0A88/$File/exercise-cumpston-report.pdf
[accessed 22 October 2010].
panflu/publishing.nsf/Content/ahmppi-2009 [accessed 22 October 2010].
22 October 2010].
New York, Columbia University School of Nursing, 2007. Available from: http://www.nycepce.org/Documents/PHEmergencyExerciseToolkit.pdf [accessed
22 October 2010].
0017/53180/HNEH_XFG_Final_Summary_Report_Dec_2008.pdf [accessed
22 October 2010].
Annals of Emergency Medicine, 2006, 48(2):194–199, e2.
doi:10.1016/j.annemergmed.2005.12.006
pmid:16953532